Tuberous Sclerosis Complex
Inhibition of Neuron Hyperexcitability In The TSC Brain May Provide A Therapeutic Option To Treat Seizures
Posted November 15, 2019
Akira Yoshii M.D., Ph.D., University of Illinois at Chicago
Tuberous Sclerosis Complex (TSC) is a rare genetic disorder characterized by non-malignant tumor growth in multiple organs. When presented in the brain, these tumors can lead to epilepsy, developmental delays, intellectual disability, and autism. TSC is caused by mutations in either the TSC1 or TSC2 gene. When functioning properly, these genes code for proteins that bind together to form a complex that negatively regulates the mammalian target of rapamycin (mTOR) pathway, altering protein synthesis, cell growth, and proliferation. mTOR inhibitors have been successfully used to treat some of the pathological processes involving the brain and other organs. However, it remains unknown which neuronal proteins mTOR regulates and how malfunctions in the TSC/mTOR pathway could result in the neurological symptoms observed in TSC.
Patients with TSC typically present with masses called tubers in their brain. These tubers interfere with normal brain development and often become a focus of seizures. Further, recent work suggests that mutations in the TSC1 and TSC2 genes also lead to abnormalities in dendritic spine formation, glutamate receptor kinetics, and synaptic plasticity and that unregulated mTOR pathways may be responsible for these defects. Dr. Akira Yoshii and his team found that there are multiple critical windows for the mTOR inhibitor treatment to correct different aspects of structural abnormalities in TSC, and the responses depend on the stage of neuronal circuit formation. These results call for an additional therapeutic target to treat neurological symptoms of TSC. For example, treatment with Vigabatrin, a drug that blocks the degradation of the inhibitory neurotransmitter GABA, reduces infantile spasms, indicating a potential imbalance between neuronal excitation and inhibition in TSC patients.
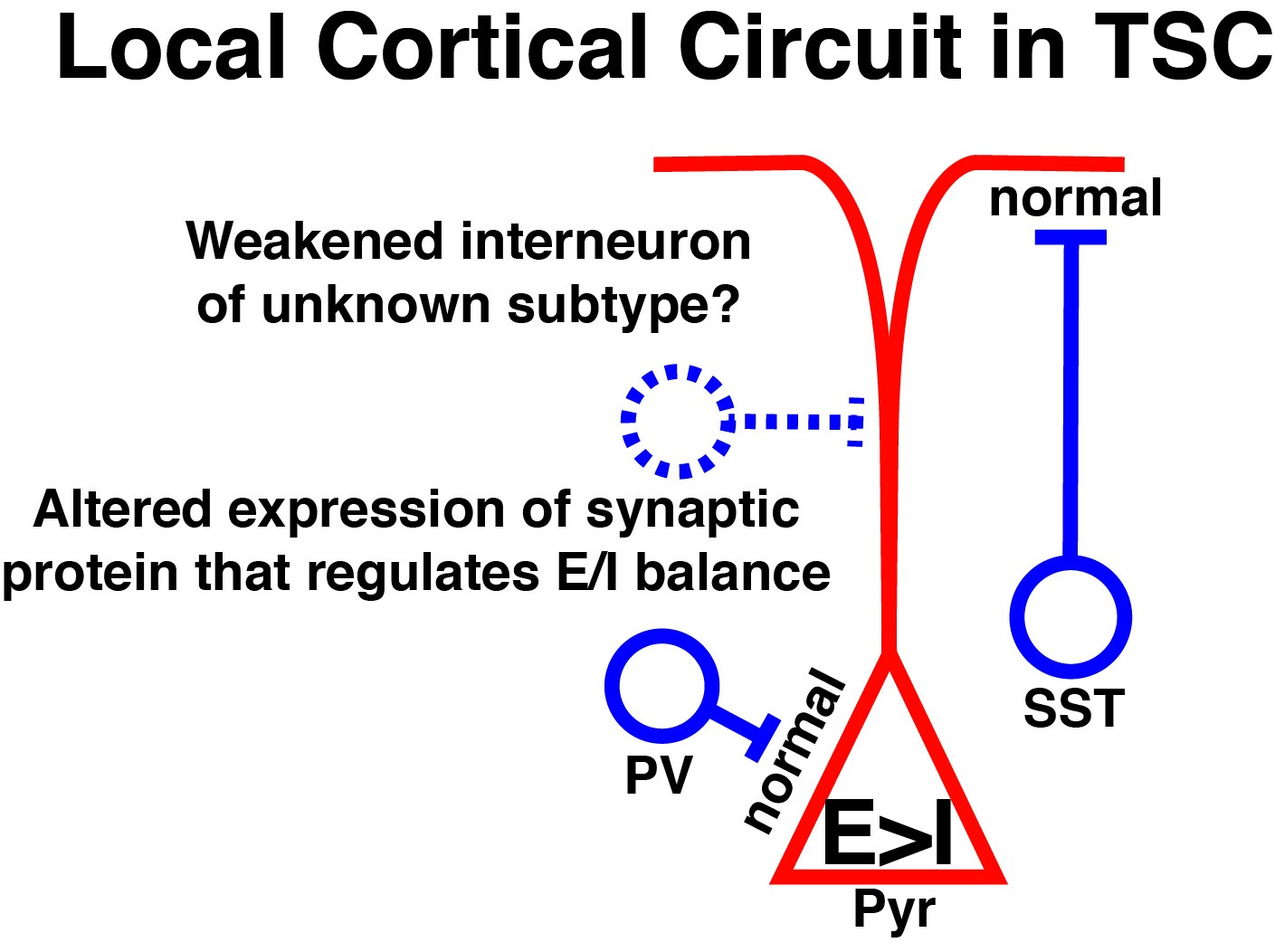
With support from a Fiscal Year 2008 Career Development Award, Dr. Akira Yoshii and his team sought to find another therapeutic target by determining if abnormal protein synthesis caused by malfunctions in the TSC/mTOR pathway triggers an imbalance in neuronal excitation and inhibition in the TSC brain. Using a mouse model with a mutation in the Tsc1 gene and gene sequencing approaches, Dr. Yoshii discovered dysregulation of more than 30 gene transcripts in the brain of mice that are deleted with theTsc1 gene. For example, the Arc protein, which mediates synaptic transmission, was decreased in the brain of mice harboring the Tsc1 gene mutation compared to mice with normal Tsc1 gene function. Dr. Yoshii rationalized that an insufficient amount of the Arc protein results in a build-up of neurotransmitter receptors at the termini of neurons, leading to hyperexcitability in Tsc1-deleted neurons. To confirm this, Dr. Yoshii and his colleagues used a biological assay capable of identifying and quantifying neurotransmitter receptors at neuronal termini. It was revealed that the ratio between excitatory AMPA and inhibitory GABA receptor subunits was biased toward hyperexcitability in Tsc1-deleted neurons. In agreement with the biochemical results, electrophysiological studies of the cortical neuronal circuit in Tsc1 mutant mice also showed evidence for hyperexcitability.
To further define hyperexcitability in TSC1 mutant neurons, Dr. Yoshii is currently using image analysis of intracellular calcium levels in Tsc1-deleted and intact neurons. Tsc1-deleted neurons showed an abnormal pattern, indicative of continual neuron activation, while non-mutant neurons exhibited both increases and decreases in calcium levels. To determine if the observed hyperexcitability in Tsc1-deleted neurons can be corrected, Dr. Yoshii treated these neurons with an inhibitor of the neurotransmitter receptor that was chosen from the list of 30 gene transcripts dysregulated by a Tsc1 deletion. Treatment of Tsc1-deleted neurons with this compound returned abnormal calcium levels to those observed in normal neurons and thus, highlighting the candidate molecule as a potential therapeutic to treat neurological symptoms of TSC.
Neurological manifestations of TSC dramatically affect a patient’s quality of life. Through Dr. Yoshii’s work, the interlocking relationship between neuronal protein synthesis and neuron hyperexcitability in the TSC brain has been revealed, leading to potential therapeutics that reduce the burden of this disease. Dr. Yoshii continues to investigate novel compounds that inhibit neuron hyperexcitability in an effort to provide multiple treatment options for patients.
Publications:
Cox R, Calderon de Anda F, Mangoubi T, and Yoshii A. 2018. Multiple critical periods for rapamycin treatment to correct structural defects in Tsc-1-suppressed brain. Front Mol Neurosci 11:409.
Zhao J and Yoshii A. 2019. Hyperexcitability of the local cortical circuit in mouse models of tuberous sclerosis complex. Molecular Brain 12:6.
Link:
Last updated Thursday, December 5, 2024














