Tuberous Sclerosis Complex
Identifying Mechanisms Initiating LAM and Angiomyolipoma in Tuberous Sclerosis Complex
Posted September 4, 2019
Magdalena Karbowniczek, M.D., Ph.D., Texas Tech University Health Sciences Center

Tuberous Sclerosis Complex (TSC) is a rare genetic disease caused by mutations in either the TSC1 or TSC2 gene. Mutations in these genes lead to neurological deficits and benign tumors in multiple organs including the brain, skin, lung (lymphangioleiomyomatosis [LAM]), heart, and kidney (angiomyolipomas). Current therapies like rapamycin, which inhibits the mTOR pathway, are effective but short-lived, resulting in tumor reoccurrence within a few months after treatment, and suggesting the involvement of non-mTOR-associated pathways in the tumorigenesis of TSC. Therefore, there is a current need in the TSC community for models that accurately reflect the tumorigenesis of peripheral TSC manifestations like LAM and angiomyolipomas.
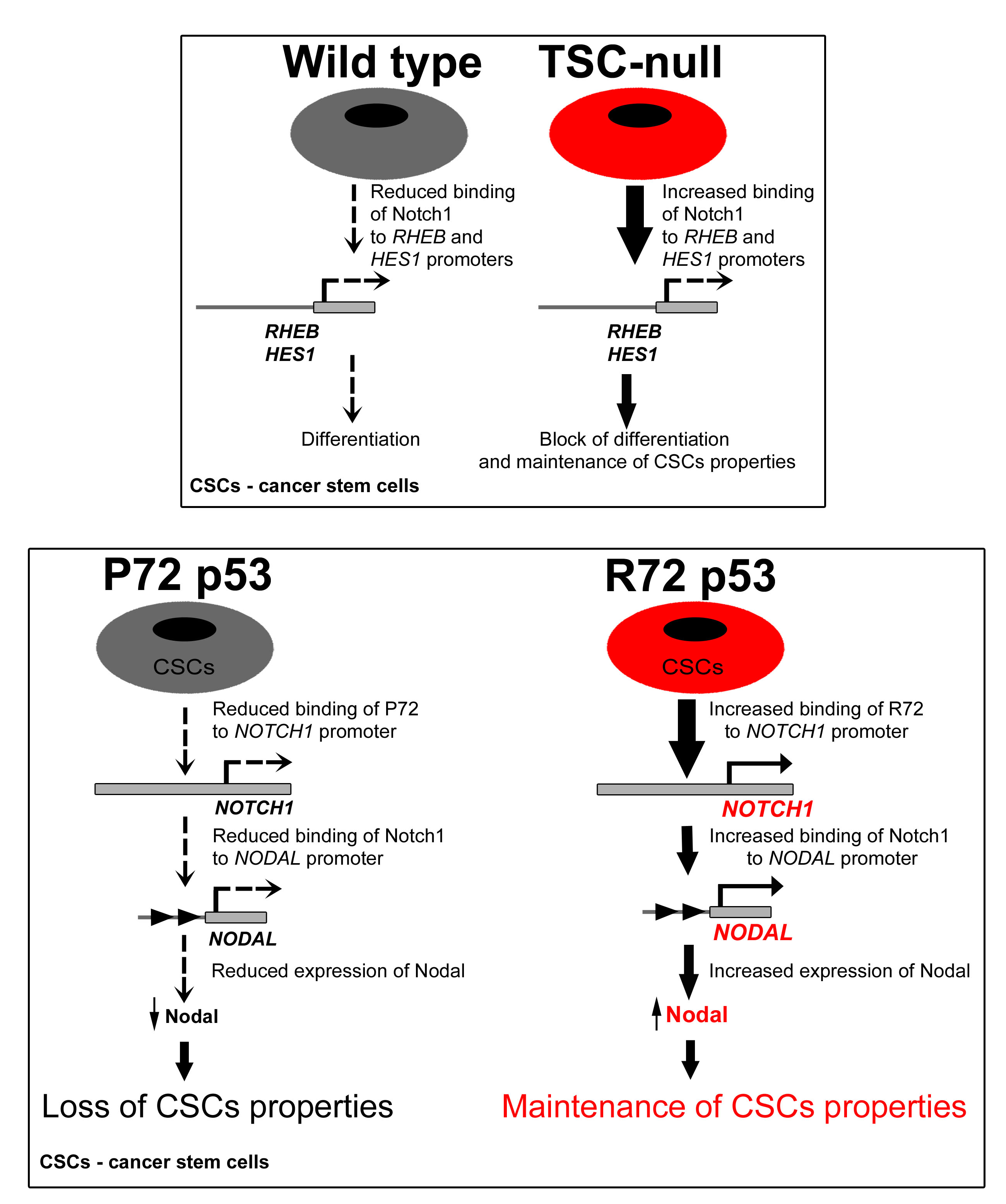
With support from a Fiscal Year 2014 Idea Development Award, Dr. Magdalena Karbowniczek sought to investigate mechanisms that are responsible for development of tumors in TSC patients with angiomyolipomas and LAM. Previously, Dr. Karbowniczek and her team showed that the Rheb/Notch pathway plays a role in TSC and angiomyolipoma formation. The Notch protein controls neuronal differentiation, proliferation, and cell migration via the p53 “cell death” pathway. Expanding upon this, Dr. Karbowniczek used novel mouse models of TSC-associated renal tumorigenesis to reveal that Notch binds directly to the Rheb gene, a previously unreported discovery, creating a Rheb-Notch-Rheb regulatory loop, which generates a pool of cancer stem cells within angiomyolipomas. Cancer stem cells are a leading cause of therapy resistance and disease spread in malignant tumors. Therapeutic disruption of the Rheb-Notch-Rheb mechanism and consequent reduction of the cancer stem cell pool in angiomyolipomas would potentially allow these tumors to be more responsive to treatments and ultimately reduce the disease burden on patients. Her most recent work demonstrated that the common TP53 polymorphism contributes to development of renal angiomyolipoma and TSC-associated renal cell carcinoma. She discovered that dysfunctional p53 causes high activation of NOTCH1 and NODAL that cooperate in TSC associated tumorigenesis.
In addition, Dr. Karbowniczek continues her work on the metastatic capabilities of LAM. She discovered while a member of Dr. Elizabeth Henske’s laboratory at the Fox Chase Cancer Center that LAM has a metastatic origin. Dr. Karbowniczek reasoned that, since exosomes (small vesicles that transport material between and within cells) play an important role in cancer metastasis, they may also contribute to LAM and other TSC manifestations. Recently, Dr. Karbowniczek showed that exosomes released from mouse cells with a mutated TSC1 gene transform normal cells into cells that behave like those with a mutated TSC1 gene. Therefore, it can be expected that cells in TSC patients that carry two mutated copies of the TSC1 or TSC2 gene can deliver mutated material to healthy cells, making them sick and thus contributing to the diverse clinical manifestations of TSC.
Tumor burden and reoccurrence dramatically affect the lives of TSC patients. Through Dr. Karbowniczek’s work, there are now newly identified mechanisms and pathways associated with LAM and angiomyolipoma formation that can potentially be targeted for therapeutic benefit. Currently, Dr. Karbowniczek and her team are exploring targeting of the exosome pathway to manage TSC manifestations. As a physician-scientist, Dr. Karbowniczek “appreciates the importance of basic and foundational studies,” but the ultimate goal of her research is to produce therapies that can be delivered to TSC patients.
Publications:
Cho J, Patel B, Bonala S, Manne S, Zhou Y, Vadrevu S, Patel J, Peronaci M, Ghouse S, Henske E, Roegiers F, Giannikou K, Kwiatkowski D, Mansouri H, Markiewski M, White B, and Karbowniczek M. 2017. Notch transactivates Rheb to maintain the multipotency of TSC-null cells. Nature Communications 8:1848.
Cho J, Patel B, Bonala S, Mansouri H, Manne S, Vadrevu S, Ghouse S, Kung C, Murphey M, Astrinidis A, Henske E, Kwiatkowski D, Markiewski M, and Karbowniczek M. 2019. The codon 27 TP53 polymorphism contributes to TSC tumorigenesis through the Notch-Nodal axis. Molecular Cancer Research, doi:10.1158/1541-7786.MCR-18-1292.
Link:
Public and Technical Abstracts: Identifying Mechanisms Initiating LAM and Angiomyolipoma in Tuberous Sclerosis Complex
Last updated Thursday, December 5, 2024














