Tuberous Sclerosis Complex
Understanding the Mechanisms of Disease Leads to Potential New Treatments for TSC-related LAM
Posted May 15, 2017
Souheil El-Chemaly, M.D., M.P.H., Brigham and Women's Hospital

Brigham and Women's Hospital
Tuberous sclerosis complex (TSC) is a genetic disorder caused by mutations to the TSC1 or TSC2 genes. Nearly 30% of women of childbearing age with TSC develop lymphangioleiomyomatosis (LAM), a rare lung disease that is characterized by the invasion of lungs by cystic tissue and is the third leading cause of TSC-related death. One of the characteristic symptoms of LAM, the development of new lymphatic blood vessels in this invading tissue, has been correlated to the expression levels of the protein vascular endothelial growth factor (VEGF)-D. Of particular interest to the understanding and treatment of LAM, VEGF-D levels have been found to correspond to disease severity and the likelihood of therapy response.
Other than this correlative link, very little was known about the role of VEGF-D in LAM or the mechanisms by which it stimulated the disease. With funding from a fiscal year 2013 Tuberous Sclerosis Complex Research Program (TSCRP) Exploration - Hypothesis Development Award, Dr. Souheil El-Chemaly at Brigham and Women's Hospital in Boston and collaborator Dr. Joel Moss at the National Institutes of Health (NIH) recently investigated the mechanisms that cause VEGF-D dysregulation in LAM. This research allowed a seamless integration of basic and translational approaches through the close collaboration of the El-Chemaly and Moss laboratories at Brigham and Women's Hospital and the NIH Intramural Research Program.
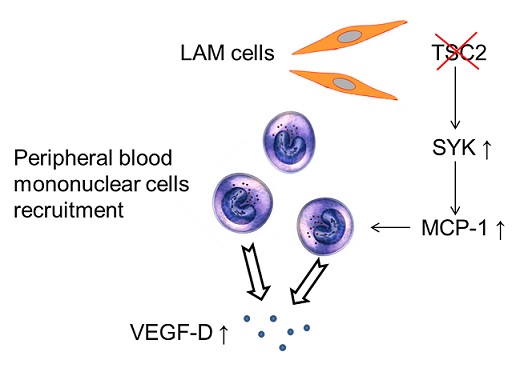
When asked to describe the motivation for his work, Dr. El-Chemaly stated, "Our main interest was to investigate the source of VEGF-D in LAM. We were puzzled by the lack of increased VEGF-D in cells that do not have the TSC2 gene. We found in cell culture and in mice that cells lacking TSC2 express a protein called MCP-1 [monocyte chemoattractant protein-1], which in turn makes immune cells produce VEGF-D." Dr. El-Chemaly and his collaborators investigated this link between MCP-1 and VEGF-D and found that spleen tyrosine kinase (SYK) plays an important role in TSC-related disease, and blocking SYK achieves the same results as blocking mTOR in mice. In other words, inhibition of SYK shrank TSC2-deficient tumors in mice, which means that tumor growth is dependent on SYK expression in LAM.
When the researchers compared SYK expression to that of MCP-1, they found that increased SYK activity results in increased production of MCP-1. Increased MCP-1 expression in cells lacking TSC2 corresponds to an increased expression of VEGF-D by immune cells, as Dr. El-Chemaly noted above. In patients with LAM, levels of VEGF-D are increased in circulating immune cells. In addition, LAM patient levels of VEGF-D correlate with levels of MCP-1. From these data, it is clear that SYK plays a key role in the development and progression of LAM and indirectly regulates VEGF-D (by way of controlling MCP-1 expression; see Figure), making it a likely therapeutic target. This is particularly exciting because SYK inhibitors are currently in advanced clinical trials for other conditions and have the potential to be an alternative, near-term therapy for LAM and TSC.
This project is a perfect example of the goals of the TSCRP Exploration - Hypothesis Development Award, which is intended to fund high-risk, high-gain science with the potential for great advances in the TSC field. Thanks to funding from the TSCRP, a potential new therapy for TSC-LAM has been identified and may be available to patients in the near future.
Reference:
Ye Cui, Wendy K. Steagall, Anthony M. Lamattina, Gustavo Pacheco-Rodriguez, Mario Stylianou, Pranav Kidambi, Benjamin Stump, Fernanda Golzarri, Ivan O. Rosas, Carmen Priolo, Elizabeth P. Henske, Joel Moss, and Souheil El-Chemaly. 2017. Aberrant SYK Kinase Signaling Is Essential for Tumorigenesis Induced by TSC2 Inactivation. Cancer Res; 77(6)
Link:
Public and Technical Abstracts: Critical Roles for SYK in Lymphangiogenesis in LAM
Last updated Wednesday, March 12, 2025














