Peer Reviewed Cancer
Boosting Listeria Hysteria: Prime Strategies Against Cancer



Posted March 22, 2022
Adam Snook, Ph.D., Thomas Jefferson University
Dr. Adam Snook
Thomas Jefferson University
Vaccine programs against infectious diseases have had substantial success due to recognition of the causative agents, known as antigens, by the immune system as "non-self." Creating vaccines against cancer becomes more difficult because of the predominant expression of a patient's 'self" antigens in the developing tumor, which utilizes host tissue that the immune system has been adapted to tolerate.1 To circumvent this issue, the use of tumor-associated antigens has offered a way to re-stimulate the immune system to target the growing tumor. The antigen-presenting cells of the immune system recognize these tumor-specific antigens and then communicate with adaptive immune cells, such as the T-cell, to produce an anti-cancer response. One of the limiting factors to producing a cancer vaccine stems from the lack of a tumor antigen expressed uniquely by the cancer and absent from normal tissue. Additionally, some cancers, such as colorectal cancer (CRC), become difficult to treat due to tumor environmental factors that produce a natural tolerance to immunotherapy.2 Therefore, finding a specific cancer antigen targeted through an immune re-stimulating delivery method would be ideal for patients with CRC.
Previously, Principal Investigator Dr. Adam Snook found a promising antigen, Guanylyl cyclase C (GUCY2C), to be a potential target for a CRC vaccine. This protein was shown to be expressed in the inner layer of the intestinal wall in both humans and mice, but more importantly, is overexpressed in CRC. The results in mice showed an activation of T-cells that specifically targeted the tumor, but not the normal tissue, meaning the antigen demonstrated immune privilege.3, 4 Immune privilege bypasses the need to target a tumor-specific antigen because the 'self" antigen is protected from autoimmunity (in which the body inflicts self-harm by its own immune system). These findings were adapted into a phase I clinical trial that demonstrated safety in humans; however, the immune response toward the tumor was limited and optimization of the vaccine was needed.5
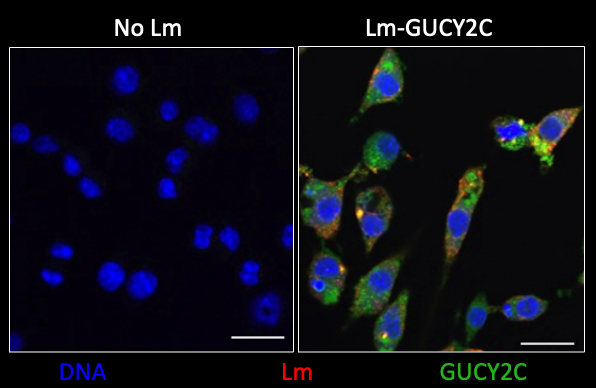
Figure 1: Image of immune cells that were untreated (No Lm) or infected with Lm-GUCY2C. Cells were then stained to reveal their nuclear DNA (blue), the Listeria (red), and GUCY2C (green).
Developing an effective delivery platform also remains a challenge for cancer vaccines. These range from bacterial and viral-based carriers to specific immune cells loaded with tumor antigens and nanotechnology. The most robust way to induce immune responses to tumor antigens has been the use of viral or bacterial delivery systems, known as vectors. Listeria monocytogenes (Lm) is a prominent example of a hopeful bacterial vector for cancer vaccines.6, 7 The ability of a patient to tolerate repeated administration to boost T-cell response, due to the lack of reinfection response to the vector by the body, makes Lm-based vectors attractive in cancer therapy, which may require re-stimulation of the immune system.
Supported by a Fiscal Year 2016 (FY16) Peer Reviewed Cancer Research Program (PRCRP) Idea Award with Special Focus, Dr. Snook leveraged the advantages of using Lm-based vectors to optimize the immune response of the GUCY2C-targeted vaccine. Using mouse models, Dr. Snook's team demonstrated that, following a priming stage from the original vaccine that faded over time, the Lm-based vector boosted and restored T-cell and immune response after multiple exposures. Furthermore, no significant toxicity or inflammation was found in the mice, illustrating that the vaccine produced results without triggering harmful autoimmunity.
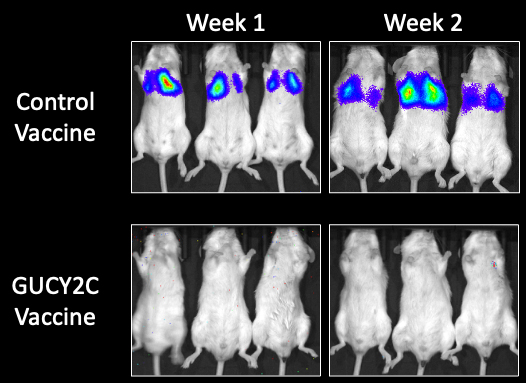
Figure 2: Image of mice with metastatic colorectal cancer in their lungs treated with control or GUCY2C vaccines. Metastatic colorectal cancer was imaged using bioluminescence imaging.
Currently, supported by a FY21 PRCRP Translational Team Science Award - Clinical Trial, Dr. Snook and clinician Dr. Bashir propose a phase I clinical trial with the GUCY2C-directed original vaccine with Lm-based vector boost for CRC patients with minimal residual disease (MRD). MRD is characterized by the presence of circulating tumor DNA. This study will test the safety and ability to induce GUCY2C-specific immune responses, overcome vector-specific immunity, and induce MRD clearance. Mouse tumor xenograft models will also be used in parallel to examine tumor immunity in patients. Interestingly, Dr. Snook and colleagues also propose the use of technology to detect circulating cell-free DNA derived from tumors, representing MRD in at-risk patients, for better surveillance and treatment selection. Among patients with stage I to III CRC who completed adjuvant chemotherapy, patients identified as circulating tumor DNA positive using the tumor-informed SignateraTM assay developed by Natera, Inc., were 17 times more likely to relapse than circulating tumor DNA negative patients.8 This MRD detection technology has been proposed as a future companion diagnostic for GUYC2C prime-boost vaccine commercialization.
CRC patients normally undergo both surgery and chemotherapy to treat their cancer. Sadly, recurring disease affects patients in all stages of CRC. Recurrence happens due to a low number of undetectable cancer cells. Only a small fraction of CRC patients benefit from conventional immunotherapy; therefore, a successful vaccine regimen will be most effective for CRC patients who are ineligible to receive other immune treatment options. CRC is the fourth most common cancer, with about 150,000 new cases per year, and is the second leading cause of cancer mortality in civilians and the military.8 These studies will create a unique opportunity for immune-based recurrence prevention in active military, Veteran, and civilian CRC populations and will pave the way toward Food and Drug Administration approval.
References:
1 Donninger H, Li C, Eaton JW, and Yaddanapudi K. 2021. Cancer vaccines: promising therapeutics or an unattainable dream. Vaccines (Basel). 9(6):668. doi: 10.3390/vaccines9060668. PMID: 34207062; PMCID: PMC8233841.
2 Bashir B and Snook AE. 2018. Immunotherapy regimens for metastatic colorectal carcinomas. Hum Vaccin Immunother. (2):250-254. doi: 10.1080/21645515.2017.1397244. Epub 2017 Dec 6. PMID: 29083978; PMCID: PMC5806658.
3 Snook AE, Stafford BJ, Li P, Tan G, Huang L, Birbe R, Schulz S, Schnell MJ, Thakur M, Rothstein JL, Eisenlohr LC, Waldman SA. 2008. Guanylyl cyclase C-induced immunotherapeutic responses opposing tumor metastases without autoimmunity. J Natl Cancer Inst. 100(13):950-61. doi: 10.1093/jnci/djn178. Epub 2008 PMID: 18577748; PMCID: PMC2749952.
4 Snook AE, Magee MS, Schulz S, Waldman SA. 2014. Selective antigen-specific CD4(+) T-cell, but not CD8(+) T- or B-cell, tolerance corrupts cancer immunotherapy. Eur J Immunol. 44(7):1956-1966. doi: 10.1002/eji.201444539. Epub 2014 May 21. PMID: 24771148; PMCID: PMC4107120.
5 Snook AE, Baybutt TR, Xiang B, Abraham TS, Flickinger JC Jr, Hyslop T, Zhan T, Kraft WK, Sato T and Waldman SA. 2019. Split tolerance permits safe Ad5-GUCY2C-PADRE vaccine-induced T-cell responses in colon cancer patients. J Immunother Cancer. 7(1):104. doi: 10.1186/s40425-019-0576-2. PMID: 31010434; PMCID: PMC6477737.
6 Gunn GR, Zubair A, Peters C, Pan ZK, Wu TC, Paterson Y. 2001. Two Listeria monocytogenes vaccine vectors that express different molecular forms of human papilloma virus-16 (HPV-16) E7 induce qualitatively different T-cell immunity that correlates with their ability to induce regression of established tumors immortalized by HPV-16. J Immunol. 167(11):6471-6479. doi: 10.4049/jimmunol.167.11.6471. PMID: 11714814.
7 Sewell DA, Shahabi V, Gunn GR 3rd, Pan ZK, Dominiecki ME, Paterson Y. 2004. Recombinant Listeria vaccines containing PEST sequences are potent immune adjuvants for the tumor-associated antigen human papillomavirus-16 E7. Cancer Res. 64(24):8821-8825. doi: 10.1158/0008-5472.CAN-04-1958. PMID: 15604239.
8 Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, and Jemal A. 2018. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 68(6):394-424. doi: 10.3322/caac.21492. Epub 2018 Sep 12. Erratum in: CA Cancer J Clin. 2020 70(4):313. PMID: 30207593.
Links:
Last updated Monday, December 15, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
