Prostate Cancer
The PROPHECY Study Validates the Use of Two AR-V7 Biomarker Assays for Predicting Hormone Therapy Resistance in Men with Metastatic Castration-Resistant Prostate Cancer



Posted April 16, 2019
Andrew Armstrong, M.D., Duke University
Duke University
Androgen receptor splice variant 7 (AR-V7) has been associated with poor clinical prognosis and hormone therapy resistance in prostate cancer patients, making it a biomarker of interest in recent years. The Prostate Cancer Research Program (PCRP) has previously featured the work of two research teams who have been working to develop biomarker assays to detect AR-V7 in circulating tumor cells (CTCs) from patients with metastatic castration-resistant prostate cancer (mCRPC).1,2 A new prospective, multicenter clinical trial, known as PROPHECY, has independently validated these non-invasive peripheral blood tests for predicting patient response and progression-free and overall survival with the standard androgen receptor signaling inhibitors (ARSi), enzalutamide and abiraterone, in men with high-risk mCRPC.3 Notably, this multi-center prospective-blinded study, led by Duke University, included additional liquid biopsy analyses of CTCs including DNA and RNA studies that will form the basis for ongoing and future publications and discoveries for men with mCRPC. This study has leveraged multiple investments by the PCRP; development of both biomarker assays was supported through separate PCRP awards, and PROPHECY was conducted through the PCRP-supported Prostate Cancer Clinical Trials Consortium (PCCTC) at 5 participating clinical research centers, which was also responsible for accelerating the clinical testing of abiraterone and enzalutamide to obtain Food and Drug Administration approval in 2011 and 2012, respectively.
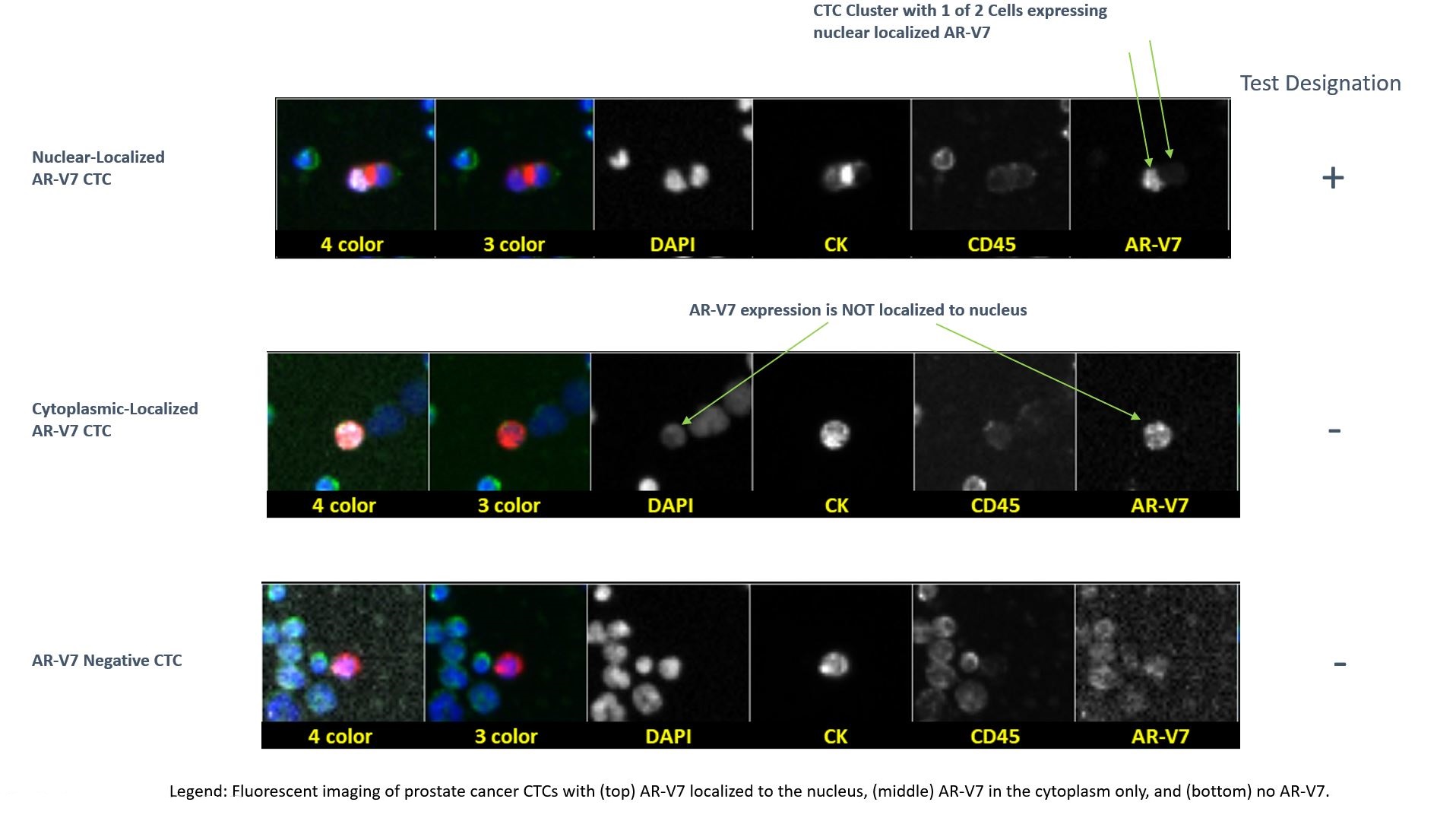
The primary goal of the PROPHECY study was to validate and compare the prognostic capabilities of AR-V7 in CTCs using the Epic Biosciences CTC nuclear-specific AR-V7 protein assay and the Johns Hopkins University modified AdnaTest CTC AR-V7 mRNA assay. The trial consisted of 118 mCRPC patients enrolled at five clinical sites, all of whom were classified as high-risk. Of these men, 55 were treated with abiraterone, 58 with enzalutamide, and 5 with both drugs concurrently. Each patient’s physician selected treatment without knowledge of their initial AR-V7 status. Additionally, laboratory personnel were blinded to the clinical results, ensuring validity of the results and lack of bias. The primary outcome of the trial was progression-free survival (PFS), and the secondary outcomes were overall survival (OS) and prostate-specific antigen (PSA) responses. There was 82% observed percentage agreement (86 of 105 patients with readable results) between the two assays. Results of the trial showed that AR-V7 detection by both tests was independently associated with shorter PFS and OS in these men. Patients with a positive baseline AR-V7 by either assay showed little clinical benefit from abiraterone or enzalutamide treatment, indicating that AR-V7 was strongly associated with hormonal therapy resistance, even after adjusting for the number of CTCs and clinical prognostic factors, and even after adjusting for the heterogeneity of CTC phenotypes.
This groundbreaking clinical trial not only showed strong clinical utility for both of these assays, but also validated AR-V7 as a specific and novel prognostic biomarker for making timely and personalized treatment decisions in patients with mCRPC. The overall finding of PROPHECY suggests that mCRPC patients with a detectable AR-V7 had a significantly poorer response to ARSi treatment than AR-V7-negative patients and should potentially be treated with taxane-based chemotherapies or an investigational therapy. Conversely, men without detectable levels of AR-V7 had a much greater probability of PSA decline, radiographic responses, and had longer PFS and OS. However, AR-V7 did not explain all of the resistance, meaning that AR-V7-negative men with mCRPC should still be followed closely with PSA and radiographic monitoring during treatment. The investigators found that some men developed new AR-V7 positive CTCs at progression, and ongoing work is characterizing the whole genomic and phenotypic changes in CTCs over time to study novel mechanisms of resistance to these AR inhibitors. The PCRP has been instrumental in providing funding for both AR-V7 assays, and the investigators were able to leverage the multi-center network of the PCRP-funded PCCTC to help validate the clinical utility of these assays at a faster rate than could be achieved by individual institutions. All of these efforts will ultimately help to better inform critical and costly treatment decisions for prostate cancer patients to potentially improve mCRPC patient survival and quality of life.
References:
Publication:
Armstrong A., Halabi S., Luo J. 2019. Prospective Multicenter Validation of Androgen Receptor Splice Variant 7 and Hormone Therapy Resistance in High-Risk Castration-Resistant Prostate Cancer: The PROPHECY Study. Journal of Clinical Oncology.
Last updated Thursday, December 5, 2024














