Prostate Cancer
Noninvasive Detection of AR-FL/AR-V7 as a Predictive Biomarker for Therapeutic Resistance in Men with Metastatic Castration-Resistant Prostate Cancer
Third feature in a 3-part series focusing on clinical advancements in personalizing AR-targeted therapy



Posted March 21, 2018
Jun Luo, Ph.D., Johns Hopkins University
Johann de Bono, M.B., Ch.B., F.R.C.P., M.Sc., Ph.D., F.Med.Sci., The Institute of Cancer Research: Royal Cancer Hospital
Stephen Plymate, M.D., University of Washington

Many patients with castration-resistant prostate cancer (CRPC) benefit from treatment with androgen receptor (AR) inhibitors, such as abiraterone and enzalutamide, although these drugs are very expensive and many patients ultimately become resistant. An abnormal splice variant of the AR, known as AR-V7, is associated with resistance to both of these drugs and poor clinical prognosis. The important link between AR-V7 levels and patient response to androgen therapies has spurred the research community to develop a commercial assay that would reliably detect AR-V7 and inform treatment decisions for men with prostate cancer. Johns Hopkins University researchers, led by Dr. Jun Luo, approached this unmet clinical need by developing a non-invasive assay that uses AdnaTest technology to isolate and detect AR-V7 in circulating tumor cells (CTCs) in the blood. With funding from a FY14 Biomarker Development Award, Dr. Luo collaborated with Dr. Stephen Plymate at the University of Washington and Dr. Johann de Bono at the Institute of Cancer Research, to validate and implement this simple blood test into the clinic.
To accomplish this goal, they prospectively enrolled 202 patients with CRPC who were starting treatment with abiraterone or enzalutamide and investigated the prognostic value of detecting AR-V7 from CTCs by categorizing the patients into three categories: CTC-, CTC+/AR-V7-, and CTC+/AR-V7+. They followed these patients for response to these therapies and found that CTC- patients had better clinical outcomes compared to CTC+ patients; and of the CTC+ patients, the presence of AR-V7 correlated to inferior outcomes. This expanded analysis characterized the importance of CTC-based AR-V7 detection in predicting outcomes in CRPC patients receiving hormone therapy, and, to the best of the investigators' knowledge, is the first to suggest that this assay should be interpreted using three separate prognostic categories.
In order to further increase the specificity of the assay and address current limitations in the precision measurement of AR-V7, Dr. Luo and colleagues improved upon the AR-V7 AdnaTest assay by using a technology named RNA in situ hybridization (RISH), which is capable of visualizing single splice junctions in cells and tissue, ultimately making the AdnaTest compatible with automated quantification of AR-V7. Using this improved assay, they generated quantitative data of full-length AR and AR-V7 in patients starting abiraterone or enzalutamide following biopsy. They correlated this data to clinical outcomes and found that positive AR-V7, but not higher levels of full-length AR, was associated with worse prognosis. These results are the first demonstration and application of a new test that utilizes the RISH technology to quantify with high specificity the detection of clinically significant levels of AR-V7 mRNA in CRPC patients.
To determine how results of incorporating the AR-V7 test would influence clinical practice, Dr. Luo's group conducted a questionnaire-based survey of providers who ordered the first 150 tests at Johns Hopkins University. Results from the survey showed that providers used AR-V7 testing to influence clinical decision making more often than not. Physicians reported that men with AR-V7+ results had the most treatment changes, which ultimately may have improved outcomes for these patients.
It was announced in 2017 that Qiagen is commercializing the AdnaTest Prostate Cancer Panel for research use to detect AR-V7 from blood samples and investigate resistance to potential drugs for CRPC. Qiagen has acquired an exclusive worldwide license from Johns Hopkins University for detecting the AR-V7 biomarker in all sample and cell types through nucleic acid tests such as polymerase chain reaction (PCR) or next-generation sequencing (NGS). Successful execution of these clinical results and ongoing clinical studies of AR-V7 RISH will have a near-term impact on patients considering treatment options for CRPC. It will help clinicians and patients make decisions that will maximize the therapeutic benefit of existing therapies in the standard-of-care setting. It is also expected that this test will help to accelerate new drug development, and this study is gaining momentum in a path toward FDA approval of the test as a drug development tool. Johns Hopkins University has already incorporated this test into a phase II clinical trial (NCT02601014) that is looking to determine how well the check point inhibitor nivolumab (anti-PD1) and the T cell regulatory CTLA4 blockade agent ipilimumab (anti-CTLA4) work in mCRPC patients who are AR-V7 positive. By using the AR-V7 RISH test, they can monitor treatment response and determine the clinical efficacy of the trial.
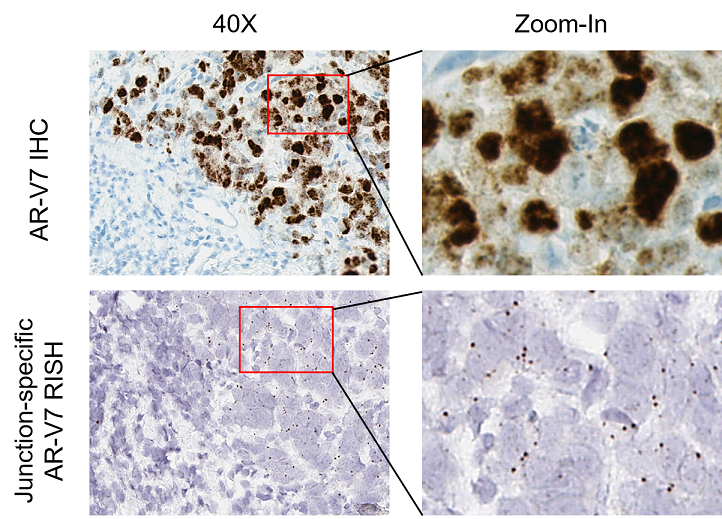
Comparison of AR-V7 signals detected by immunohistochemistry (IHC) and BaseScope RNA in situ hybridization (RISH) in a metastatic CRPC biopsy. Adjacent sections prepared from the same specimen containing both AR-V7 positive and AR-V7 negative regions were processed for AR-V7 IHC (top) and RISH (bottom).
Publications:
Markowski MC, Silberstein JL, Eshleman JR, et al. 2017. Clinical Utility of CLIA-Grade AR-V7 Testing in Patients With Metastatic Castration-Resistant Prostate Cancer, JCO Precision Oncology.
Zhu Y, Sharp A, Anderson CM, et al. 2017. Novel Junction-specific and Quantifiable In Situ Detection of AR-V7 and its Clinical Correlates in Metastatic Castration-resistant Prostate Cancer European Urology 302838 (17) 30695.
Antonarakis ES, Lu C, Brandon L, et al. 2017. Clinical Significance of Androgen Receptor Splice Variant-7 mRNA Detection in Circulating Tumor Cells of Men With Metastatic Castration-Resistant Prostate Cancer Treated With First- and Second-Line Abiraterone and Enzalutamide, J Clin Oncol. 35(19):2149-2156.
Lokhandwala PM, Riel SL, Haley L, et al. 2017. Analytical Validation of Androgen Receptor Splice Variant 7 Detection in a Clinical Laboratory Improvement Amendments (CLIA) Laboratory Setting.The Journal of Molecular Diagnostics 19(1): 115-125.
Luo J. 2016. Development of AR-V7 as a putative treatment selection marker for metastatic castration-resistant prostate cancer Asian Journal of Andrology 18, 580:585
Antonarakis ES, Armstrong AJ, Dehm SM, et al. 2016. Androgen receptor variant-driven prostate cancer: Clinical implications and therapeutic targeting. Prostate cancer and prostatic diseases 19(3):231-41.
Link:
Last updated Monday, March 10, 2025














