Tick-Borne Disease
A Pre-Exposure Immunoprophylaxis for the Prevention of Lyme Disease



Posted October 6, 2021
Yang Wang, Ph.D., MassBiologics, University of Massachusetts Medical School

For many of us, enjoying time outdoors includes hiking, taking our kids to the park, going for long walks with the dog, and having barbeques with family and friends. Before walking out the door we grab our keys, some water, and maybe slather on some sunscreen, but how many of us stop to think about putting on permethrin-treated clothes, wearing long pants, or applying bug repellent? Benjamin Franklin said, “an ounce of prevention is worth a pound of cure,” and that is certainly true for tick-borne diseases (TBDs) for which rapid, sensitive, and specific diagnostic assays are lacking and treatments options are limited.
Lyme disease is the most common TBD and the most common vector-borne disease in the United States, and while the true rate of infection is underestimated due to many cases going undiagnosed, misdiagnosed, or unreported, the CDC recently estimated that 476,000 Americans are diagnosed and treated for Lyme disease annually.1 For some patients, treatment with antibiotics, such as doxycycline, is effective and leads to a full recovery, while other patients may develop more persistent symptoms and receive a diagnosis of Post-Treatment Lyme Disease Syndrome (PTLDS).2 Unfortunately, patients who go undiagnosed or misdiagnosed or whose treatment fails are at risk for additional complications, as Borrelia burgdorferi, the predominant Lyme disease-causing bacteria, can spread and result in Lyme arthritis (inflammation of the joints), carditis (inflammation of the heart), neuroborreliosis (infection of the central nervous system), and other conditions involving multiple other organ systems, including the placenta of pregnant women.3,4
The Tick-Borne Disease Research Program (TBDRP), managed by the Congressionally Directed Medical Research Programs (CDMRP), engages with patients, their advocates, and other stakeholders to ensure that their voices are heard when developing program areas of focus. As such, TBD prevention is one of the four main Focus Areas of the TBDRP.
When we think of infectious disease prevention, vaccines and good hygiene practices typically come to mind. However, Dr. Yang Wang from MassBiologics, University of Massachusetts Medical School, and her team of experts have taken a different approach, developing a preventative measure for Lyme disease called a pre-exposure immunoprophylaxis or PrEP. Administering neutralizing antibodies to prevent severe illness has been effective for other infectious diseases, so Dr. Wang and her team hypothesized that they could improve upon one of their human monoclonal antibodies (HuMab) that they previously identified as being specific for the outer surface protein A (OspA) of Borrelia burgdorferi. Ideally, the modified HuMab PrEP candidate would retain its superior borreliacidal (Borrelia burgdorferi-killing) activity and possess an extended half-life, thus stabilizing antibody blood concentrations and preventing Lyme disease for a longer period of time. First, the optimal OspA HuMab, called 2217, was selected based on maximal borreliacidal activity in vitro and in murine studies. Then, HuMab 2217 was modified (HuMab 2217LS), to successfully double its half-life in mice and in non-human primates (NHPs) (Figure 1).5 When assessed for borreliacidal activity, as compared to HuMab 2217, HuMab 2217LS was slightly less potent against B. burgdorferi cultures in vitro,5 but provided a similar level of protection to mice in a tick challenge model of B. burgdorferi infection (Figure 2).5
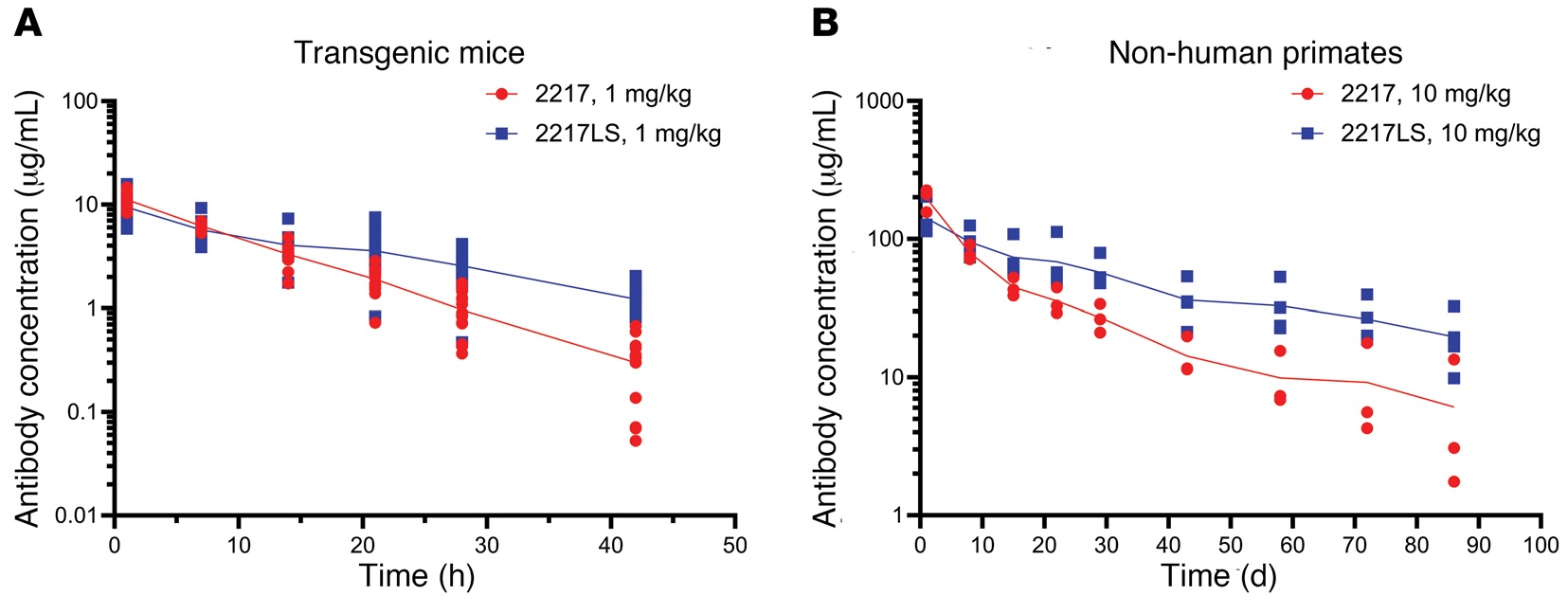
Figure 1: Modification of HuMab 2217 increases the stability of the antibody in animals. HuMab 2217 (parental human OspA monoclonal antibody; red circles) and the modified HuMab 2217LS (extended half-life OspA HuMab; blue squares) in the serum of (A) transgenic mice (n=16/group) and (B) NHPs (n=4/group). Overall there was a 2-fold increase in the half-life of the antibody in both studies.
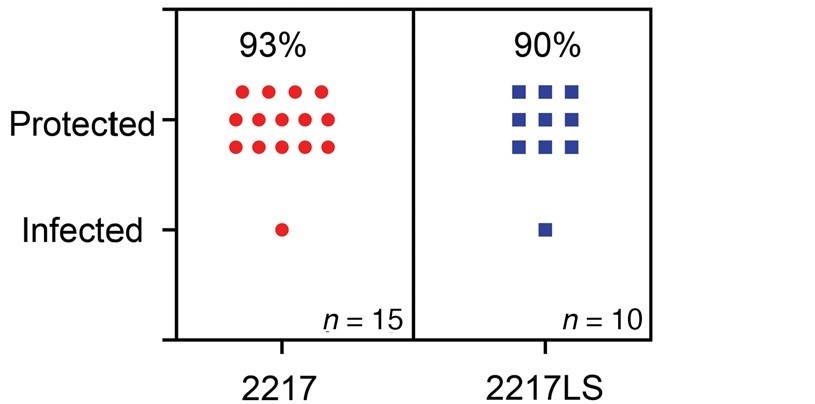
Figure 2: HuMab 2217 and the extended half-life 2217LS protect mice from tick transmission of Borrelia burgdorferi. Mice were administered 5 mg/kg of either 2217 or 2217LS and challenged with B. burgdorferi-infected nymphal ticks. Efficacy was determined by evaluating tissue biopsies for the presence of bacterial growth or DNA and by assessing seroconversion (the presence of Borrelia-specific antibodies).
To further assess the protective efficacy of the extended half-life HuMab 2217LS, Dr. Wang collaborated with a team of investigators, including Dr. Monica Embers at Tulane University and colleagues at Biomere, to implement an NHP tick-transmission model that mimics human Lyme disease.5,6 In these studies, NHPs were administered different doses of HuMab 2217LS (ranging from 3 mg/kg to 90 mg/kg) or an irrelevant human antibody (10 mg/kg) and then challenged with 20 B. burgdorferi-infected ticks. Serum was sampled throughout the study to assess seroconversion (development of anti-B. burgdorferi antibodies) via an enzyme-linked immunosorbent assay (ELISA) specific for antibodies against a synthetic peptide that reproduces the sequence of an invariable region of a B. burgdorferi surface protein, called C6. NHPs also underwent skin biopsies, which were evaluated for the presence of B. burgdorferi using bacterial culture. Of 19 NHPs that received 2217LS, only 1 animal was positive by B. burgdorferi culture while, as expected, all 3 of the irrelevant antibody controls were positive for B. burgdorferi infection. Consistent with the culture results, only 1 animal in the 2217LS-treated group was positive by ELISA and all others were protected from Borrelia infection (Figure 3).5 The C6 ELISA data were confirmed using a multiplexed array that evaluates seroconversion in response to other B. burgdorferi antigens. As expected, no antibody response was detected for 18 out of 19 HuMab 2217LS-treated animals, demonstrating protection from B. burgdorferi infection. Negative control animals that received the irrelevant antibody all showed an antibody response as expected, proving that protection was specific to the HuMab 2217L.5 Considering all data, Dr. Wang and her team concluded that 83%-100% of NHPs were protected from B. burgdorferi infection, depending on the concentration of the HuMab 2217LS administered.
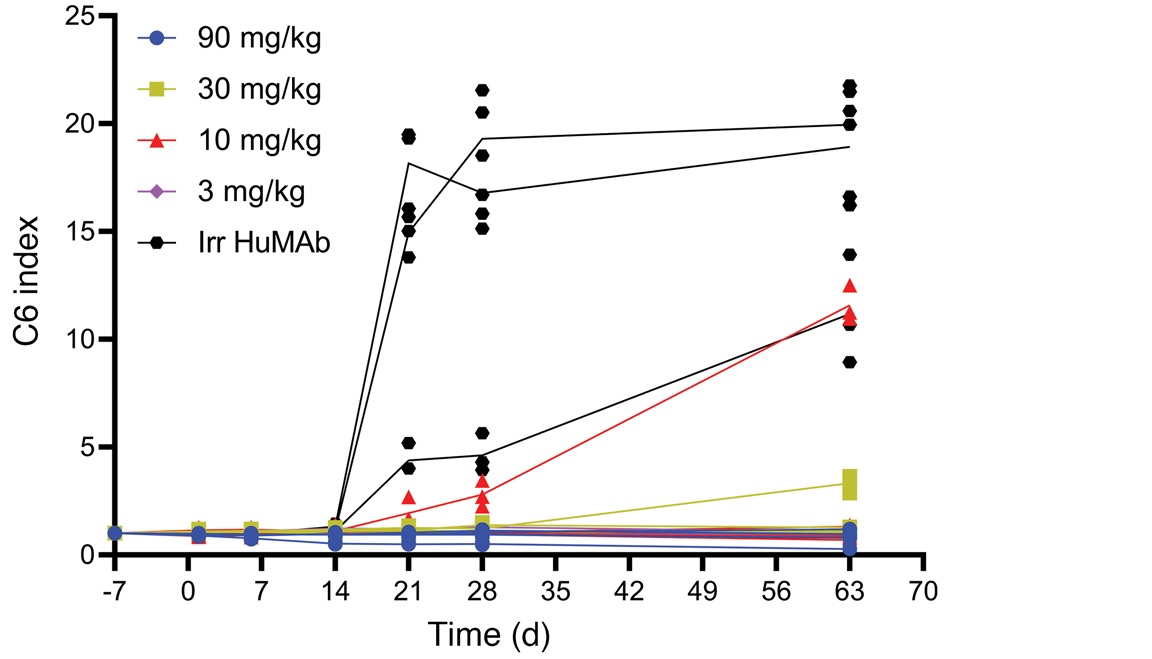
Figure 3: 2217LS blocks the transmission of Borrelia burgdorferi in the tick-challenge NHP model of infection. HuMab 2217LS was administered (3 mg/kg-90 mg/kg) to NHPs and serum from each animal was collected at timed intervals following antibody administration. NHPs were challenged with B. burgdorferi-infected ticks and the presence of antibodies against the C6 peptide were measured by ELISA and compared with those in the irrelevant antibody (10 mg/kg)-treated control group. Note that the C6 ELISA is specific to antibodies against a portion of the VlSe lipoprotein of B. burgdorferi and therefore, the assay is a measure of the seroconversion that occurs after infection. All but one 2217LS-treated animal were protected from B. burgdorferi transmission, as indicated by little/no anti-C6 antibodies. These results were confirmed using ELISAs for other B. burgdorferi antigens.5
In summary, Dr. Wang and her team have demonstrated that this extended half-life HuMab, 2217LS can prevent tick transmission of B. burgdorferi to mice and NHPs. Currently, there are no Food and Drug Administration (FDA)-approved human vaccines to prevent Lyme disease, and prevention strategies rely on physical barriers and the use of tick repellents, which require compliance and reapplication. For our Service Members, permethrin-treated uniforms are the primary line of defense against tick bites and unfortunately, potency wanes over time with washing.7 Therefore, the idea that a single dose of a human antibody PrEP can be administered once before the onset of peak tick season is attractive and would benefit Service Members, their beneficiaries, and the American public. While it may not protect from other TBDs, for those living, working, or recreating in areas with high incidence of Lyme disease or robust tick populations, or for those who just desire another layer of protection, this PrEP could provide another barrier to B. burgdorferi infection and reduce the incidence of Lyme disease.
Notably, the results from this TBDRP-funded effort have helped to advance Dr. Wang and MassBiologics' PrEP candidate along the pathway to FDA approval, with an investigational new drug (IND) application approved this year and a Phase I clinical trial (NCT04863287) underway for HuMab 2217LS.
Citations:
1 https://www.cdc.gov/lyme/data-research/facts-stats/index.html
4 https://www.cdc.gov/lyme/data-research/facts-stats/index.html
5 Schiller ZA, Rudolph MJ, Toomey JR, Ejemel M, LaRochelle A, Davis SA, Lambert HS, Kern A, Tardo AC, Souders CA, Peterson E, Cannon RD, Ganesa C, Fazio F, Mantis NJ, Cavacini LA, Sullivan-Bolyai J, Hu LT, Embers ME, Klempner MS, and Wang Y. 2021. Blocking Borrelia burgdorferi transmission from infected ticks to nonhuman primates with a human monoclonal antibody. J Clin Invest. 131(11):e144843. doi: 10.1172/JCI144843. PMID: 33914704. PMCID: PMC8159683.
6 Embers ME, Grasperge BJ, Jacobs MB, and Philipp MT. 2013. Feeding of ticks on animals for transmission and xenodiagnosis in Lyme disease research. J Vis Exp. (78):50617. doi: 10.3791/50617. PMID: 24022694. PMCID: PMC3857350.
Link:
Last updated Thursday, January 8, 2026
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
