Reconstructive Transplant Research
Researching New Ways to Block Inflammation and Prevent Severe Tissue Damage Following Transplantation



Posted October 12, 2022
Christene A. Huang, Ph.D., University of Colorado
 Christene A. Huang
Christene A. Huang
(Photo Provided)
For patients who have sustained complex or severe injuries that leave them with structural, functional, and/or aesthetic deficiencies, vascularized composite allograft (VCA) transplantation may be a beneficial treatment option. VCA is the transfer of vascularized body parts that contain multiple tissue types such as skin, muscle, bone, nerves, and blood vessels (e.g., a face or a hand) to a recipient who has suffered a severe injury. After a VCA graft has been procured from a donor, the graft is no longer receiving oxygen and other nutrients via blood flow, a condition called ischemia. Once the graft is transplanted, circulation is restored in a process called reperfusion. Following prolonged ischemia, there is a high risk of additional severe tissue damage post-reperfusion, which results from dysregulated inflammation and contributes to graft rejection. Although there have been many advances in the VCA field, transplantation is complicated by limited ex vivo preservation times due to the risk of ischemia reperfusion injury (IRI), and transplant rejection remains a challenge.
Dr. Christene Huang, a plastic and reconstructive surgery and transplant surgery professor from the University of Colorado, received a Fiscal Year 2018 (FY18) Reconstructive Transplant Research Program (RTRP) Concept Award to investigate new approaches to combat inflammation and IRI during VCA transplantation. Dr. Huang and her team studied the role of Galectin-3 (Gal3) in VCA IRI, since this protein has been shown to be involved in the transition to chronic inflammation in many diseases, such as cancer, arthritis, heart disease, and autoimmune diseases. They established a rat hind-limb transplant model in which donor limbs were stored at 4oC for 6 or 24 hours prior to transplant, allowing severe IRI to occur.
Dr. Huang's team used their new model to test the effect of blocking Gal3 in hind-limb recipients starting 7 days prior to transplant through the end of the experiment at 6 days post-transplant, using modified citrus protein (MCP) provided through drinking water. The team found that rats treated with Gal3 inhibitor had significantly reduced inflammatory response to ischemic injury post reperfusion compared to untreated rats (Figure 1C). In addition, circulating Gal3 protein levels in untreated rats were significantly increased compared to rats treated with Gal3 inhibitor (Figure 1A-B).
To build on these findings, Dr. Huang received an FY21 RTRP Advanced Technology Development Award, where she will investigate Gal3 as a potential non-invasive biomarker for monitoring VCA graft rejection. This aligns well with the RTRP's priority of advancing reliable non-invasive monitoring of VCA graft rejection. Together, Dr. Huang's studies will help us to better understand IRI after VCA and may lead to improved strategies for reducing inflammation and improving outcomes after transplantation.
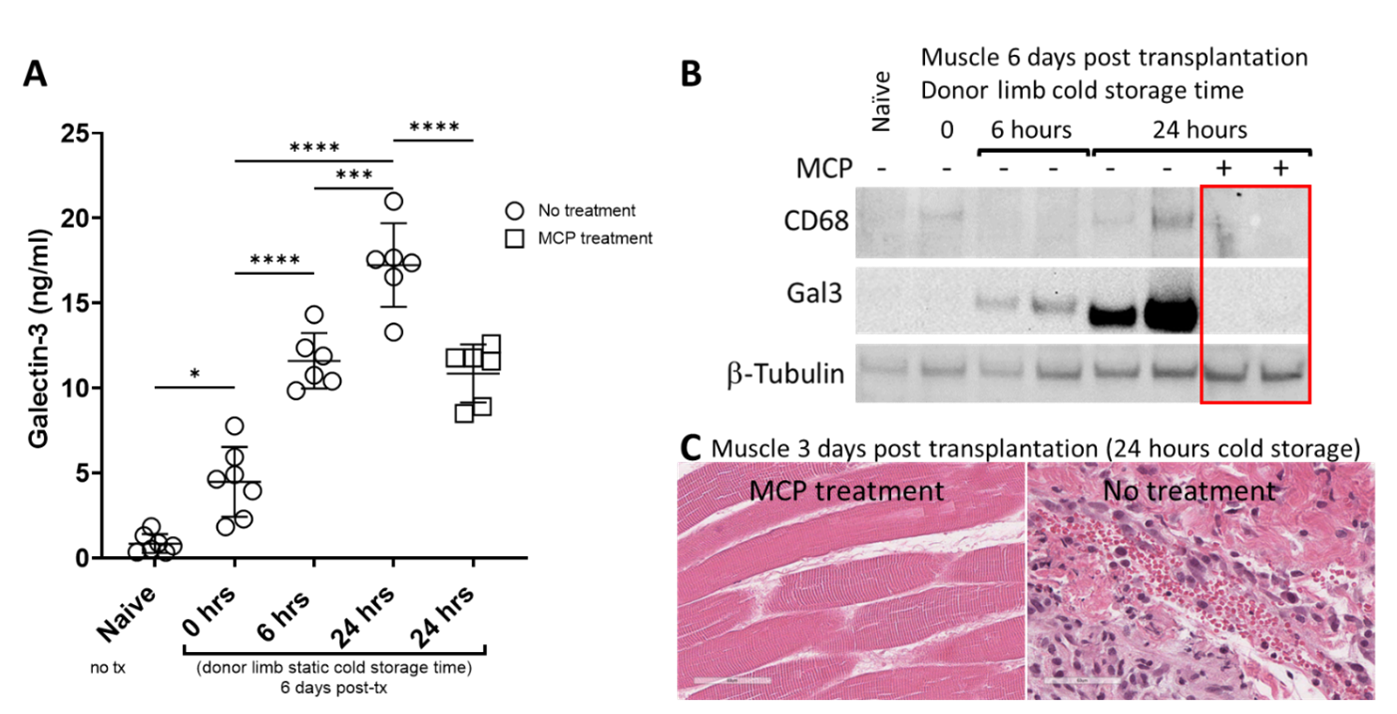
Figure 1: Galectin-3 is increased in circulation (A) and donor muscle tissue (B) in recipient rats transplanted with hind limbs subjected to prolonged cold storage. Blocking galectin-3 with modified citrus pectin (MCP) reduced circulating galectin-3 levels (A) and prevented galectin-3 upregulation and CD68 macrophage infiltration in the donor muscle post-transplant (B). Significantly reduced inflammation was confirmed by H&E (40X) of donor muscle from MCP treated (left panel) vs untreated (right panel) recipients (C).
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
