Reconstructive Transplant Research
Mapping the Inflammatory Response to Vascularized Composite Allotransplantation



Posted December 17, 2021
Dr. Yoram Vodovotz, University of Pittsburgh
Dr. Vijay Gorantla, Wake Forest University
For catastrophically injured individuals, hand and/or face transplantation may be a viable option for restoring quality of life and function. These types of transplants are called vascularized composite allotransplantation or VCA: "vascularized" due to the presence of blood vessels for the circulation of blood and essential nutrients to the hand or face graft; "composite" referring to the different tissue types within the graft, such as skin, muscle, nerve, blood vessels, and bone; and "allotransplantation," meaning transplanted from one individual to another. Over 165 VCA procedures have been performed worldwide, demonstrating the feasibility of this treatment option.1 Following the surgical transplant procedure, VCA recipients must remain on drugs to regulate the immune system and prevent transplant rejection. This is similar to solid organ transplant recipients; however, the composite nature of VCA complicates this immune regulation. Each of the tissue types in the graft elicits a unique immune response, with the skin being particularly immunogenic, often triggering a strong immune response.
 Dr. Yoram Vodovotz
Dr. Yoram Vodovotz
 Dr. Vijay Gorantla
Dr. Vijay Gorantla
Dr. Vodovotz at the University of Pittsburgh, together with Dr. Vijay Gorantla at Wake Forest University, received a fiscal year 2014 award to better understand the interactions of different VCA tissue types with the immune system. They sought to unravel these interactions using a systems biology approach. Systems biology is a scientific approach to unravel complex interactions by looking at the big picture. For example, if you were trying to investigate traffic congestion, a systems approach would look at the whole highway network instead of focusing on a single street on a city map. By analyzing 27 proteins known to mediate in the inflammatory process, the team was able to develop maps of the key immunological processes driving the immune response following VCA.2
Specifically, the team used a rat model of VCA to perform hind-limb transplants between immunologically matched donor-recipient pairs (i.e., rats with the same immune genes) and mismatched donor-recipient pairs (i.e., rats with different immune genes, increasing the chance of graft rejection). For mismatched recipients, animals were given tacrolimus, the most commonly used immunosuppressive drug in VCA. Blood, skin, and muscle samples were collected over 20 days, and the protein expression of the 27 inflammatory mediators was analyzed. Through statistical and computational analysis, the team was able to build maps of inflammatory networks from the skin, muscle, and blood samples that identified distinct immune mediators in each tissue type following VCA. For VCA recipients receiving tacrolimus treatment, the key inflammatory mediators were inter-leukin-1 alpha (IL-1 alpha) in the skin; leptin and vascular endothelial growth factor (VEGF) in muscle samples; and leptin, lipopolysaccharide-induced CXC chemokine (LIX), and monocyte chemoattractant protein 1 (MCP-1) in peripheral blood.2 By integrating the skin and muscle data, the team was able to define interactions between tissue types, and thus created a "virtual VCA." The addition of the peripheral blood response to the muscle and skin data generated an "in silico" or "virtual animal" model. This analysis suggests a complex inflammatory interaction after VCA in the presences of tacrolimus, with leptin as the primary driver. Control VCA, transplanted between matched donor-recipient pairs without tacrolimus treatment, had fewer inflammatory mediators involved (Figure 1).
This computational and systems biology approach to defining the hallmarks and functional mediators of inflammation in VCA transplantation can help identify markers for early detection and targeted treatment of acute rejection. The team will next perform computational analysis of the inflammatory profile using archived human hand transplant patient samples.
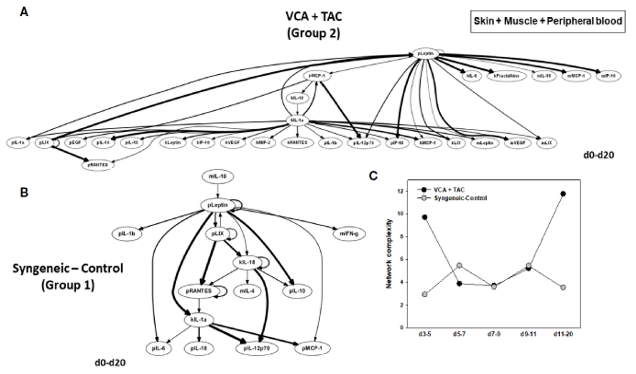
Figure 1: Differential inflammatory network patterns in rats undergoing VCA +TAC vs. Syngeneic Control. LEW rat recipients received full MHC-mismatched BN limbs with TAC (1 mg/kg/day, i.p.) until post-operative day 20, followed by drug withdrawal. LEW rat recipients that received MHC-matched LEW limbs without TAC served as control. Peripheral blood, skin and muscle tissue samples were collected at 0, 3, 5, 7, 9, 11, and 20 days and assayed for 27 inflammatory mediators using the rat multiplex Luminex assay followed by Dynamic Bayesian Network (DyBN) analysis. Panels (A, B) show the DyBNs for skin, muscle, and peripheral blood (combined) in VCA + TAC and Syngeneic-Control, respectively.
References:
1Jacoby A, Cohen O, Gelb B.E., Ceradini D.J., Rodriguez ED. 2021. Vascularized Composite Allotransplantation and Immunobiology: The Next Frontier. Plastic and Reconstructive Surgery . June, Volume 147, Issue 6, pp. 1092e-1093e. doi: 10.1097/PRS.0000000000007954.
2Aral AM, Zamora R, Barclay D, Yin J, El-Dehaibi F, Erbas VE, Dong L, Zhang Z, Sahin H, Gorantla VS, and Vodovotz Y. 2021. The Effects of Tacrolimus on Tissue-Specific, Protein-Level Inflammatory Networks in Vascularized Composite Allotransplantation. Front. Immunol. 12:591154. doi: 10.3389/fimmu.2021.591154.
Link:
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
