Reconstructive Transplant Research
Improving Ischemia Reperfusion Injury in Vascularized Composite Tissue Allotransplantation via Histone Deacetylase Modulation



Posted August 29, 2018
Matthew H. Levine, M.D., University of Pennsylvania
Vascularized composite allotransplantation (VCA) is a reconstructive surgery that transplants multiple tissue types from a deceased donor as a functional unit, such as a hand or face, in order to restore function and offer improved aesthetic outcomes. Despite the success of the approximately 150 VCA procedures performed worldwide, widespread use of VCA as a treatment option for patients suffering significant traumatic injury has been limited. This is due in part to the extreme difficulty in finding matching donors. Unlike solid organ transplants, such as a kidney or heart, the external nature of the VCA graft requires careful matching of size, gender, skin tone, and age, in addition to blood type and immunological compatibility. Further limiting the potential donor pool is the irreversible tissue damage, called ischemia reperfusion injury (IRI) that develops as a result of cold preservation and lack of blood flow to the graft following procurement. The current standard of care limits this storage time to approximately 6 hours, reducing the potential donor pool to those within geographic vicinity of the recipient. Development of strategies to extend the amount of time that a graft can remain viable following cold storage will allow improved access to VCA for both military Veterans and civilians living with limb loss or severe craniofacial injuries.
Dr. Matthew Levine and his team received a Fiscal Year 2015 Idea Discovery Award to investigate ways to improve graft preservation through the use of drug inhibitors targeting histone deacetylases (HDACs). HDACs are responsible for regulating gene expression by modulating gene accessibility, and inhibition of these proteins has been shown to increase the tolerance of kidney transplants to cold storage in mouse models. Now Dr. Levine is translating this approach to mouse models of ischemia and VCA transplantation. Using a tourniquet-based warm model of ischemia injury, mice were treated with HDAC inhibitors 16 hours prior, and again 30 minutes prior, to limb ischemia, and muscle injury was assessed by histology. In this model, treatment with an inhibitor that targets all HDACs (TSA) led to significantly less tissue injury compared to control treated mice (p<0.05; see Figure 1). This protective effect was even greater when the HDAC-6 specific inhibitor, Tubastatin A (TubA), was used (p<0.01), while use of an HDAC-1 specific inhibitor (MS275) did not protect from ischemia injury (Figure 1).
Dr. Levine's team is currently performing a cold ischemia model of mouse hind limb transplantation using the HDAC inhibitors that have shown promise in the warm ischemia model. These experiments will help to further determine the role of HDAC inhibition in promoting ischemia tolerance. Strategies that serve to improve graft preservation will be instrumental to increasing the accessibility of VCA to patients with significant traumatic injuries and lessening wait times for donor/recipient matches.
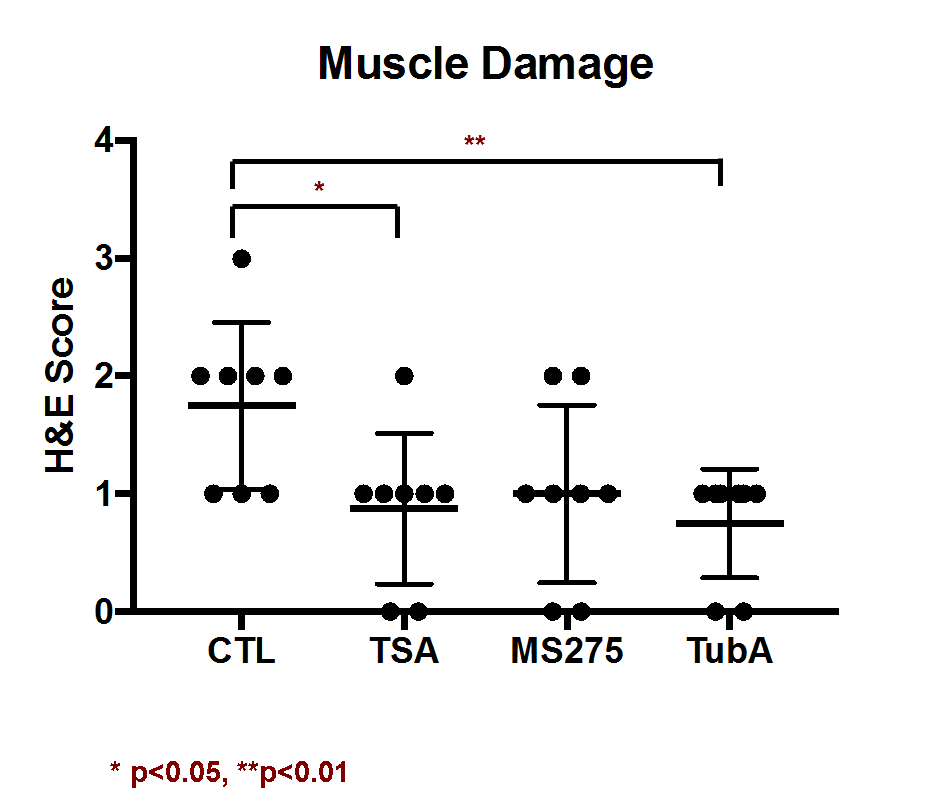
Figure 1. Muscle damage after warm IRI after TSA and Tubastatin A (TubA) treatment was mitigated significantly compared to control or MS-275 treatment groups (the asterisks represent significance).
Last updated Friday, December 13, 2024














