Reconstructive Transplant Research
T-Regulatory Cell-Based Therapies Promote Survival of Vascularized Composite Allografts



Posted May 8, 2018
Wayne W. Hancock, M.D., Ph.D., Children's Hospital of Philadelphia
Catastrophic tissue loss is an unfortunate reality for numerous combat Soldiers injured from gunshot wounds and improvised explosive devices. The general public are also susceptible to tissue loss from traumatic injuries, malignancies, and congenital malformations. A potential solution is vascularized composite allotransplantation (VCA), which is a surgical procedure that can replace large sections of composite tissue (i.e., tissue units that include bone, nerve, muscle, vasculature, and skin, such as a hand or a face) by transplanting the same tissue units from a deceased donor. Although an estimated 7 million people nationwide could benefit from these life changing procedures, VCA has been limited to approximately 150 procedures worldwide due, in part, to the requirement for lifelong immunosuppression therapy to prevent allograft rejection. Cumulative exposure to immunosuppression is associated with significant risks, including infection, organ toxicity, diabetes, and tumor formation.
Dr. Wayne Hancock, of the Children's Hospital of Philadelphia, is building on promising data in the organ transplant field that could ultimately lead to the elimination of immunosuppression after VCA. He hypothesizes that a subpopulation of immune cells, called T-regulatory cells (Tregs), can provide protective anti-rejection effects following VCA. Tregs are central to establishing and maintaining immune tolerance, because they suppress the effects of other T cells that activate the immune response and participate in transplant rejection. Tregs expressing the transcription factor Foxp3 (Foxp3+ Tregs) are key to immune tolerance and depend on the interleukin-2 (IL-2) signaling molecule for survival. Dr. Hancock received a fiscal year 2015 Reconstructive Transplant Research Program Idea Discovery Award to investigate whether Foxp3+ Treg-based therapies are capable of prolonging allograft survival in mouse models of VCA.
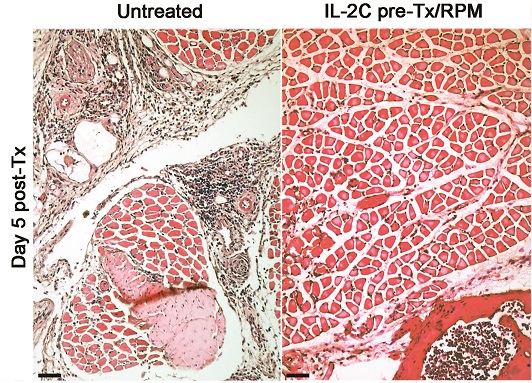
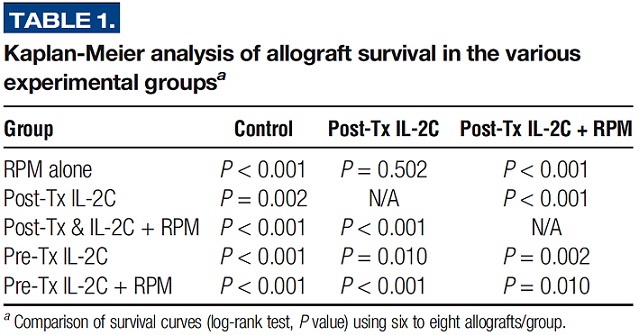
Dr. Hancock and his team found that administering an IL-2/anti-IL-2 monoclonal antibody complex (IL-2C) to naive mice resulted in a 10-fold increase in the number of Foxp3+ Tregs. When applied before or after forelimb transplantation in a mouse model of VCA, IL-2C therapy significantly prolonged allograft survival from 7 days in control mice treated with saline alone to more than 21 days in mice treated with IL-2C to expand the Treg population (p<0.001, Table). An added benefit was achieved with the combination of pre-transplant IL-2C therapy with post-transplant rapamycin administration, which led to greater than 50 days of VCA survival (p<0.001 compared to saline-treated controls, Table). Comparison of the histology of the forelimb allografts in the first week post-engraftment revealed signs of Grade III rejection in untreated control mice, whereas allografts from mice that received pre-transplant IL-2 therapy combined with rapamycin post-transplant showed no signs of rejection (Figure), which was maintained until 6 weeks post-transplant. This finding is likely the result of increased numbers of Tregs, as both IL-2C and rapamycin support the expansion of this specific population of T cells. This work illustrates the potential for Foxp3+ Treg-based therapies to serve as an alternative approach for immune system modulation and as an anti-rejection strategy.
In ongoing experiments, Dr. Hancock's team is further exploring the role of Tregs in promoting VCA survival through the inhibition of histone deacetylases, which is known to promote both the production of Tregs and their functions. Novel approaches that minimize exposure to immunosuppression in VCA while protecting recipients from rejection will help to increase the number and successful outcomes of VCA procedures. Wider acceptance and use of VCA will enable improved quality of life for Service members and civilians who have sustained otherwise irreparable tissue injury and loss.
Publication:
Xu H, Dahiya S, Wang L, Akimova T, Han R, Zhang T, Zhang Y, Qin L, Levine MH, Hancock WW, and Levin LS. 2018. Utility of IL-2 Complexes in Promoting the Survival of Murine Orthotopic Forelimb Vascularized Composite Allografts. Transplantation. 102(1):70-78.
Reference:
1Gander B, Brown CS, Vasilic D, et al. 2006. Composite Tissue Allotransplantation of the Hand and Face: A New Frontier in Transplant and Reconstructive Surgery. Transpl Int. 19(11):868-880.
Link:
Technical and Lay Abstracts: Peritransplant Treg-Based Immunomodulation to Improve VCA Outcomes
Last updated Wednesday, March 12, 2025














