Reconstructive Transplant Research
Developing Therapeutic Reagents to Accelerate the Rate of Peripheral Nerve Growth after Reconstructive Transplantation



Posted November 9, 2018
Samantha J. Butler, Ph.D., University of California, Los Angeles

Peripheral nerve damage is commonly associated with extremity wounds, which accounted for 54% of all injuries sustained in the conflicts in Afghanistan and Iraq.1 Some of these injuries involve devastating damage to, or the complete loss of, hands or limbs as a result of explosive device detonation. Reconstructive transplantation, also known as vascularized composite allotransplantation (VCA), is a surgical procedure which serves to replace the lost tissue with a fully functional equivalent from a deceased donor. This procedure offers recipients the prospect of maximal aesthetic and functional restoration; however, achieving this ideal outcome is still fraught with many challenges, such as the need for long-term immunosuppression and the slow and unpredictable regeneration of injured peripheral nerves. Dr. Samantha Butler and her team at the University of California Los Angeles received a Fiscal Year 2015 Idea Discovery Award to investigate these two challenges.
For a VCA procedure to be considered successful, a number of factors must fall into place. Two of the most critical factors of success are graft acceptance by the recipient's immune system and regeneration of peripheral nerves to reinnervate the transplanted graft. Reinnervation is required for the recipient to regain full function after transplant. To promote graft acceptance and prevent rejection, the standard treatment is to suppress the normal function of the immune system. However, little is known about how the required immune suppression effects nerve regeneration and reinnervation of the graft. Dr. Butler and her team have sought to determine the effects of several different immunosuppressants on nerve regeneration in a mouse model.
Following surgical nerve transection, mice were treated with one of three different immunosuppressants (FK506, cyclosporinA [CsA], or rapamycin). Nerve regeneration was then assessed by immunofluorescence using the markers neurofilament, which labels all nerve axons, and GAP43, whose expression increases during regenerative axon growth (Figure 1). After 7 days of recovery post-nerve transection, there was robust nerve regeneration in all groups (Figure 1). Quantification of GAP43 expression revealed a trend toward higher levels of this marker beyond the lesion site in animals treated with the immunosuppressant CsA, while FK506 and rapamycin treatment did not lead to significant differences in axon regeneration. The potential role of CsA in promoting nerve regeneration was further supported by staining for cofilin, a protein which leads to an increased rate of axon growth when active. Seven days after nerve transection, the levels of inactive cofilin in CsA-treated mice were lower than those in FK506 and control treated mice and were more similar to levels seen at day 0 post-transection. This suggests that cofilin may be more active in CsA-treated mice supporting the observation that CsA-treated nerves had improved regeneration.
Dr. Butler is now focusing efforts on the identification of novel compounds that can increase the rate of nerve regeneration without compromising a patient's immune system. Such a drug would have the potential to improve the recovery time for an estimated 20 million Americans who suffer from peripheral nerve injury caused by trauma or medical disorders.2 Using high throughput imaging, over a thousand compounds will be screened for their ability to increase the length of nerves extending from stem cell-derived human spinal motor neurons. New drugs that can improve the rate of nerve regeneration will help both Veterans and the public recover from peripheral nerve damage and improve graft function for VCA recipients.
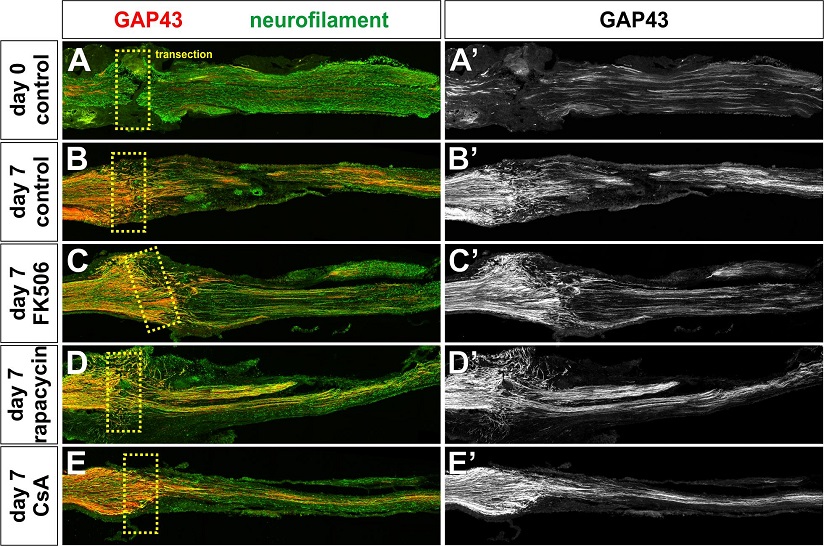
Figure 1. GAP43+ axon regeneration following immunosuppression. Mice were either (1) immediately fixed after transection (n=3 mice, day 0, A) or (2) permitted to recover for 7 days (n=12, day 7, B-E). During this period, mice were mock injected (n=3, B) or treated with 5mg/ml FK506 (n=3, C), rapamycin (n=3 D) or cyclosporinA (n=3, E). The nerves were processed for immunohistochemistry, thin-sectioned and labeled with antibodies against GAP43 (red, A-E, A-E) or neurofilament (green, A-E). A dotted box indicates the position of the transection.
References:
1 Owens BD et al. 2007. Characterization of Extremity Wounds in Operation Iraqi Freedom and Operation Enduring Freedom. J Orthop Trauma. Article 17414553. https://doi.org/10.1097/BOT.0b013e31802f78fb
2 Grinsell D and Keating CP. 2014. Peripheral Nerve Reconstruction after Injury: A Review of Clinical and Experimental Therapies. BioMed Res Int. Article 25276813. http://dx.doi.org/10.1155/2014/698256.
Link:
Last updated Wednesday, March 12, 2025














