Peer Reviewed Orthopaedic



Posted January 11, 2022
Zongbing You, M.D., Ph.D.
Professor and Vice Chair for Research
Department of Structural and Cellular Biology
Tulane University School of Medicine
 Dr. Zongbing You
Dr. Zongbing You
Osteoarthritis is the degradation of cartilage in the joint which can cause pain, loss of motion, and eventually disability. This disease is the most common form of arthritis and affects over 32.5 million people each year according to the Centers for Disease Control and Prevention. Veterans are specifically susceptible to osteoarthritis as it impacts them twice as much as civilians, 26.9 to 12.4 per 1000 people respectively. 1 Current treatment for osteoarthritis requires multiple surgeries, as donor tissue must be harvested from a healthy part of the joint, cultured, and then implanted. 2 Therefore, there is a need to simplify the overall procedure.
Dr. You and his team at Tulane University have been working with modified human adipose-derived stromal/stem cells (ASCs) for implantation in preclinical models to help treat osteoarthritis. To create this implant, the original ASCs are isolated from human fat collected during liposuction procedures, which are cultured and grown to form a pellet of cells that is later used for implantation. One of the exciting aspects of Dr. You's work is the ability to modify the ASCs' genetic code to express doublecortin (DCX), which has been shown to promote ASCs to become chondrocytes that express markers of authentic articular chondrocytes (e.g., growth differentiation factor 5 and matrilin 2). 3 Thus, implanting this pellet derived from the modified cells into the damaged cartilage may improve cartilage healing without the use of multiple surgeries or donor specific tissue.
With Fiscal Year 2014 funding from the Peer Reviewed Orthopedic Research Program (W81XWH-15-1-0444), Dr. You has taken this work a step further. His group has tested these modified ASCs in rabbits and monkeys and recently published their results in a high-impact journal npj Regenerative Medicine. In this work (Figure 1), a defect or hole in the cartilage was created in the femoral trochlear groove (the area underneath the kneecap on the femur), and then the pellet was implanted for 6, 12, or 24 months and evaluated for cartilage repair. Three groups were used to test the effect of DCX: fibrin as a negative control to fill the void, DCX-ASCs, and ASCs alone as a direct comparison. For the rabbits, all histological endpoints (6, 12, and 24 months) showed that the DCX-ASCs had an increased histological score compared to the ASCs alone or fibrin. For the monkeys, the macroscopic and histological scoring at 24 months was increased in the DCX-ASCs compared to ASCs alone or fibrin. These results suggest that ASCs with DCX may repair cartilage better than ASCs alone. Thus, implants with the modified ASCs into a patient with osteoarthritis may promote better healing and avoid multiple surgical procedures, the potential of which awaits more preclinical validation and clinical testing.
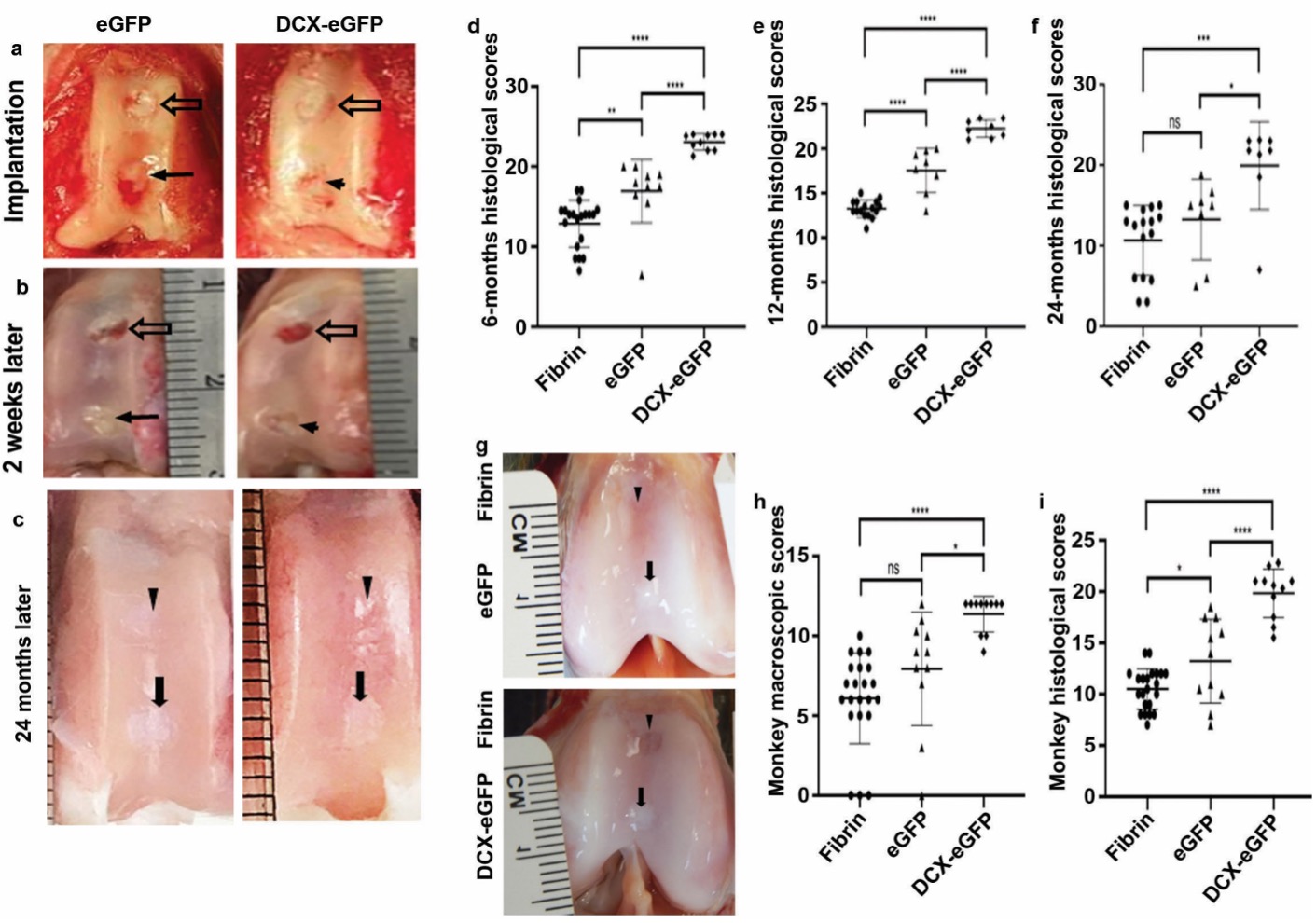
Figure 1. Summary of the main results of the W81XWH-15-1-0444 project. a Representative pictures of cartilage defects (holes) in the rabbit knee cartilage at the time of pellet implantation surgery. The upper hole was filled with fibrin (negative control); the lower hole was filled with either enhanced green fluorescence protein (eGFP) pellets (ASCs alone) or DCX-eGFP pellets (DCX-ASCs) for comparison. b Representative pictures of the cartilage defects at 2 weeks after surgery; the upper fibrin-filled hole was almost empty; the lower hole was still filled with pellets. c Representative pictures of the rabbit cartilage defects repaired at 24 months after surgery; the upper fibrin-filled hole was repaired with fibrous tissue under microscopic examination; the lower pellets-filled hole was repaired with cartilage under microscopic examination. d-e Histological scores of rabbit cartilage repair at 6, 12, and 24 months after surgery, showing that DCX-ASCs group had significantly better scores than ASCs alone or fibrin group. g Representative pictures of the monkey cartilage defects repaired at 24 months after surgery; the upper fibrin-filled hole was repaired with fibrous tissue under microscopic examination; the lower pellets-filled hole was repaired with cartilage. h Macroscopic scores of monkey cartilage repair at 24 months after surgery, showing that DCX-ASCs group had significantly better score than ASCs alone or fibrin group. i Histological scores of monkey cartilage repair at 24 months after surgery, showing that DCX-ASCs group had significantly better score than ASCs alone or fibrin group. The scoring was done according to the criteria of International Cartilage Repair Society (ICRS).
Future studies may include testing of the strategy in repair of larger cartilage defect size in large animals such as goats/sheep, increasing the number of animals used to strengthen the preclinical data, modification of how DCX is incorporated into the ASCs, and assessing the mechanical properties of the repaired cartilage. If successful, this new strategy may provide better cartilage repair for millions of Veterans, Service Members, and civilians diagnosed with osteoarthritis.
Publication:
Ge D, O'Brien MJ, Savoie FH, Gimble JM, Wu X, Gilbert MH, Clark-Patterson GL, Schuster JD, Miller KS, Wang A, Myers L, You Z. Human adipose-derived stromal/stem cells expressing doublecortin improve cartilage repair in rabbits and monkeys. NPJ Regen Med. 2021 Nov 30; 6(1):82. doi: 10.1038/s41536-021-00192-6.
References:
1 Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. 2011. Incidence of physician-diagnosed osteoarthritis among active duty United States military service members. Arthritis Rheum. 63(10):2974-2982.
2 McGowan KB, Stiegman G. 2012. Regulatory challenges for cartilage repair technologies. Cartilage. 4(1):4-11.
3 Ge D, Zhang QS, Zabaleta J, Zhang Q, Liu S, Reiser B, Bunnell BA, Braun SE, O'Brien MJ, Savoie FH, You Z. 2014. Doublecortin may play a role in defining chondrocyte phenotype. Int J Mol Sci. 15(4):6941-6960.
Links:
Last updated Monday, January 5, 2026
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
