Peer Reviewed Orthopaedic



Posted July 5, 2022
 Dr. Amos Winter, Massachusetts Institute of Technology
Dr. Amos Winter, Massachusetts Institute of Technology
Summary: Cutting-edge prosthetic feet continue to push the boundaries of what was once considered possible. Individuals with limb loss can run, jump, and return to daily life with the help of assistive devices. However, the costs of some of the technologically advanced prosthetic devices limit their reach. The concept of low-cost plastic medical devices is not new. However, prosthetists and design engineers need additional information in order to ensure that a plastic prosthetic foot will optimize outcomes for their individual patients. With funding from the Peer Reviewed Orthopaedic Research Program (PRORP), Dr. Amos Winter and Dr. Victor Prost from Massachusetts Institute of Technology, and Dr. Matthew Major from Northwestern University created an algorithm for clinicians to create low-cost, plastic prosthetic feet that are customized to a patient's body weight and size to induce desired walking biomechanics. In a limited clinical trial, five below-knee amputees were asked to choose their preferred prosthetic foot among three options: their own prosthetic foot, an energy-storing prosthetic foot, and a low-cost, plastic, passive foot designed using their algorithm. Each research participant preferred the personalized plastic prosthesis over the energy-storing prosthesis and on par with their own foot. This early clinical data suggests a potential avenue to improve amputees'quality of life by providing personalized, plastic prosthetic feet that can be manufactured and sourced at much lower costs than existing products.
Technical Details: The number of individuals living with lower-limb amputation is steadily increasing with 37 million people currently affected in the world.1 With a growing population of lower-limb prosthesis users, there is also a growing population of individuals who experience a decreased quality of life secondary to using a prosthesis. Amputees face considerable challenges to everyday mobility,2 including increased walking effort, social stigmas, and higher incidence of injuries relative to able-bodied individuals.3 Current prosthetic foot technology can provide improvements to the user's prosthetic gait and experience, compared to the traditional Solid-Ankle Cushioned Heel (SACH) prosthetic foot. However, current energy-storing prosthetic feet can cost thousands of dollars, whereas SACH feet cost tens of dollars.4 The high cost of the newest prosthetic feet make them far less accessible to users, despite their benefits. Access to affordable, high-performance, energy-storing prosthetic feet is needed to positively impact prosthesis users and improve their quality of life. Dr. Winter and his research team at the Massachusetts Institute of Technology sought to find an answer by creating a user-specific, low-cost, and mass-manufacturable energy-storing foot made of Nylon plastic. With the help of a Fiscal Year 2016 PRORP Applied Research Award, Dr. Amos Winter, his co-investigator Dr. Matthew Major, and former doctoral student, Dr. Victor Prost, created a clinical algorithm that enables the geometry and stiffness of a prosthetic foot to be tuned for a specific patient size and mass. Using this algorithm, low-cost plastic, patient-customized prosthetic feet were fabricated and evaluated.
Dr. Winter's aim to design single-component prosthetic feet that are optimized for various activities of daily living began with developing a clinical algorithm. The team devised a novel optimization metric for prosthetic foot design called, the Lower Leg Trajectory Error (LLTE), which provides a quantitative connection between the stiffness and geometry of a prosthetic foot and its anticipated biomechanical performance. Their efforts improved on a previous framework (defined by Olesnavage5) to include the entirety of the stance phase by adding the critical phases of heel strike and late stance. This algorithm, called the LLTE framework, uses baseline able-bodied Ground Reaction Force (GRF) and kinematic values, scales them to match a specific patient's size and mass, and then uses the adjusted GRFs and kinematics to create a prosthetic foot with customized stiffness and geometry that best replicates the desired biomechanics. Figure 1 provides a snapshot of the design framework and the myriad shapes possible for energy storing prosthetic feet designed for various body weights and sizes.
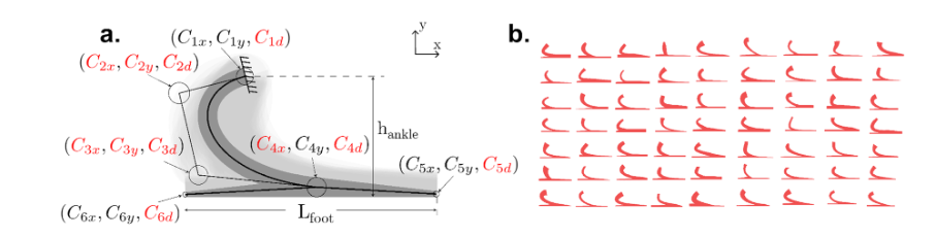
Figure 1. Overview of the LLTE framework applied in the sagittal plane. (a) The prosthetic foot parametric model, shown here overlaid on the foot design space, is defined using the wide Bezier curves' variables Cij, build height hankle, and foot length Lfoot. The design space shown in light grey was created by varying each one of the 11 independent design variables shown in red. (b) Sampled prosthetic foot shapes from the design space.
Able-bodied gait data were collected from individuals performing valuable activities such as walking quickly, up and down stairs, and on slopes. These data were used as inputs to the LLTE framework to create a foot that provides a high level of functional mobility. The optimized prosthetic feet were fabricated as a single component from Nylon 6/6 plastic using a waterjet. The performance of these plastic feet and how well they matched theoretical predictions were then evaluated during flat-ground gait testing.
Five below-knee amputees participated in the flat-ground walking tests utilizing three different prosthetic feet: their daily use prosthetic foot, the Horizon LT Foot (College Park Industries), and the study-designed LLTE foot. Results showed that the LLTE designed feet quantitatively and predictively replicated the able-bodied lower-leg kinematics and kinetics on average (within 13.9 percent for kinetic data and 5.2 percent for kinematic data). The LLTE feet more closely matched the physiological rollover shapes and reduced load on the intact limb, compared to the other two prosthetic feet. This load reduction on the contralateral limb was depicted in the data by smaller vertical ground reaction forces on the intact leg. The data also reflect an increase in energy return and peak push-off power in the LLTE feet (62 percent and 31 percent higher compared to the Horizon LT and daily-use feet, respectively). However, regardless of the prosthetic foot type, all participants walked with similar walking speeds, stance time symmetry, step width, and trunk sway range of motion. At the end of the data collection sessions, all participants filled out a survey regarding their satisfaction of the three prosthetic feet they utilized. The survey results indicated that all participants scored the LLTE foot higher than the Horizon LT foot, and two participants scored the LLTE foot higher than their daily-use foot.
Dr. Winter's research demonstrates that the newly developed LLTE framework enables the quantitative and predictive design of passive prosthetic feet, which provides similar or improved benefits compared to currently available energy-storing prosthetic feet. Further studies will be needed to explore this promising LLTE-based clinical algorithm for prosthetic foot design. These early results suggest the newly developed LLTE framework could be used to design patient-specific, high-performance, energy-storing feet using low-cost materials, such as Nylon plastic.
Publications and other Research Outcomes:
Prost V, Johnson WB, Kent JA, Major MJ, Winter AG 5th. 2022. Biomechanical evaluation over level ground walking of user-specific prosthetic feet designed using the lower leg trajectory error framework. Sci Rep. 12(1):5306. doi: 10.1038/s41598-022-09114-y. PMID: 35351910; PMCID: PMC8964743.
References:
1 World Health Organization. 2017. World Report on Disability: Standards for prosthetics and orthotics technical report.
2 Gailey R, Allen K, Castles J, Kucharik J, and Roeder M. 2008. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 45:15:29. https://doi.org/10.1682/JRRD.2006.11.0147 .
3 Zidarov D, Swaine B, and Gauthier-Gagnon C. 2009. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch Phys Med Rehabil. 90:634:645. https://doi.org/10.1016/j.apmr.2008.11.003 .
4 Andrysek J. 2010. Lower-limb prosthetic technologies in the developing world: A review of literature from 1994-2010. Prosthet Orthot Int. 34:378:98. https://doi.org/10.3109/03093646.2010.520060 .
5 Olesnavage KM, Prost V, Johnson WB, and Winter, Amos G V. 2018. Passive prosthetic foot shape and size optimization using lower leg trajectory error. J Mech Des Trans. ASME 140 102302. https://doi.org/10.1115/1.4040779.
Last updated Monday, January 5, 2026
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
