


Posted October 15, 2014
Joan Sanders, Ph.D., University of Washington, Seattle, Washington
 Soldiers who have sustained combat-related limb amputation often undergo changes in residual limb size over time. For example, these soldiers might find their prosthesis fits tightly and is difficult to put on in the morning, while late in the day it feels loose and unstable, making it not only hard to walk, but also increasing the risk of injury. Dr. Joan Sanders from the University of Washington recognized the need to develop a non-invasive instrument that could maintain a proper prosthetic socket fit. Satisfying this need will alleviate undue suffering and enhance the quality of life for wounded warriors.
Soldiers who have sustained combat-related limb amputation often undergo changes in residual limb size over time. For example, these soldiers might find their prosthesis fits tightly and is difficult to put on in the morning, while late in the day it feels loose and unstable, making it not only hard to walk, but also increasing the risk of injury. Dr. Joan Sanders from the University of Washington recognized the need to develop a non-invasive instrument that could maintain a proper prosthetic socket fit. Satisfying this need will alleviate undue suffering and enhance the quality of life for wounded warriors.
If physicians had the ability to track volume changes in a patient's prosthesis socket, then they could better fit patients with artificial limbs. With funding from a Fiscal Year 2009 Peer Reviewed Orthopaedic Research Program Technology Development Award, the University of Washington team set out to ease the discomfort that amputees often feel inside a prosthetic socket by developing a bioimpedance analysis system. Utilizing the same technology as a body fat analysis machine, this system continuously monitors the residual limb fluid volume as a patient wears the prosthesis and conducts a variety of activities over the course of a day. Dr. Sanders and her team test the system by asking patients to go through a routine that includes sitting, standing, and walking while fluid changes are recorded.
To better adjust for changes in limb volume, Dr. Sanders collaborated with Sandia National Laboratories to develop "Bladder-Liners," which are prosthetic liners that contain adjustable liquid level bladders to facilitate fluid volume stabilization. These Bladder-Liners were favorably received by all amputee subjects in a small pilot study. Additionally, she enhanced the bioimpedance analysis system to create a small, battery-powered waist-belt pack unit, called the MI-Z. The MI-Z continuously monitors patients in their regular day-to-day activities outside of a laboratory environment. Data obtained to date suggests the system shows promise and it should advance the understanding of limb fluid volume and the factors that affect it. Dr. Sanders hopes that MI-Z units can be provided to clinics treating wounded warriors to allow practitioners to incorporate limb fluid volume change data into individuals' rehabilitation treatment design in addition to the prosthetic design and fitting.

An amputee subject wearing the MI-Z portable bioimpedance system. The lightweight instrumentation box is mounted on a waistbelt worn by the subject. Thin wires extend to electrodes on the residual limb in the socket.
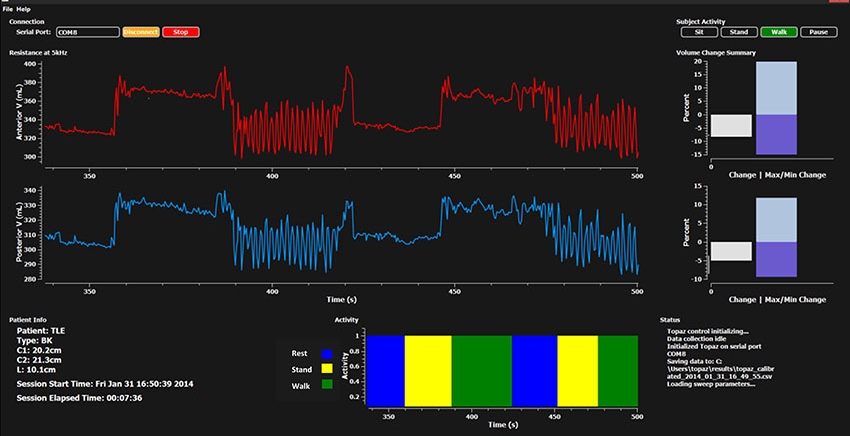
Sample data presentation from the MI-Z showing limb fluid volume change over time for the anterior and posterior regions of an amputee subject's residual limb (red and blue plots). The bar graph at the bottom shows the activities conducted (rest, stand, and walk) over the course of the same test segment. The white bar graph at the right indicates the fluid volume change since the outset of the session, and the blue bar graph shows the range. These data presented in real time help a practitioner understand a patient's fluid volume fluctuation patterns.
Links:














