Peer Reviewed Medical
Growth-Adaptive Pediatric Heart Valves: Addressing a Critical Unmet Need for Infants and Young Children That Saves Lives and Reduces Surgeries



Posted July 29, 2022
Corin Williams, Ph.D., The Charles Stark Draper Laboratory, Inc.
Congenital heart disease (CHD) is a serious condition that affects approximately 44,000 babies (1%) born each year in the U.S. One in four babies born with CHD dies before turning one year of age.1 Heart valve defects, which are common in children with CHD, contribute to severe disease and require surgical intervention.2 Despite the high mortality rate for children with CHD, there is no current clinical standard for valve replacement in children younger than age five. The only option available for many clinicians is to implant adult-sized valves that often function improperly because they are too large for young children. In the event that a smaller artificial valve is available, it is only beneficial for a short period of time, because the child's heart will continue to grow, rendering the valve obsolete.
By the time a child with CHD reaches adulthood, they will have undergone an average of three to five surgeries, creating an urgent need for pediatric heart valves that will expand as the child continues to mature.

Corin Williams, Ph.D.,
The Charles Stark Draper Laboratory, Inc.
(Photo Provided)
With support from a Fiscal Year 2019 Technology/Therapeutic Development Award through the Peer Reviewed Medical Research Program, Dr. Corin Williams and her team at the Charles Stark Draper Laboratory are working to develop a pediatric device to reduce the number of open heart surgeries infants and young children suffering from CHD will have to endure.
The Low-force Expanding/Adaptable Pediatric (LEAP) Valve is designed to adapt and expand as the child ages, thus decreasing the total number of valve replacements needed and dramatically improving quality of life.
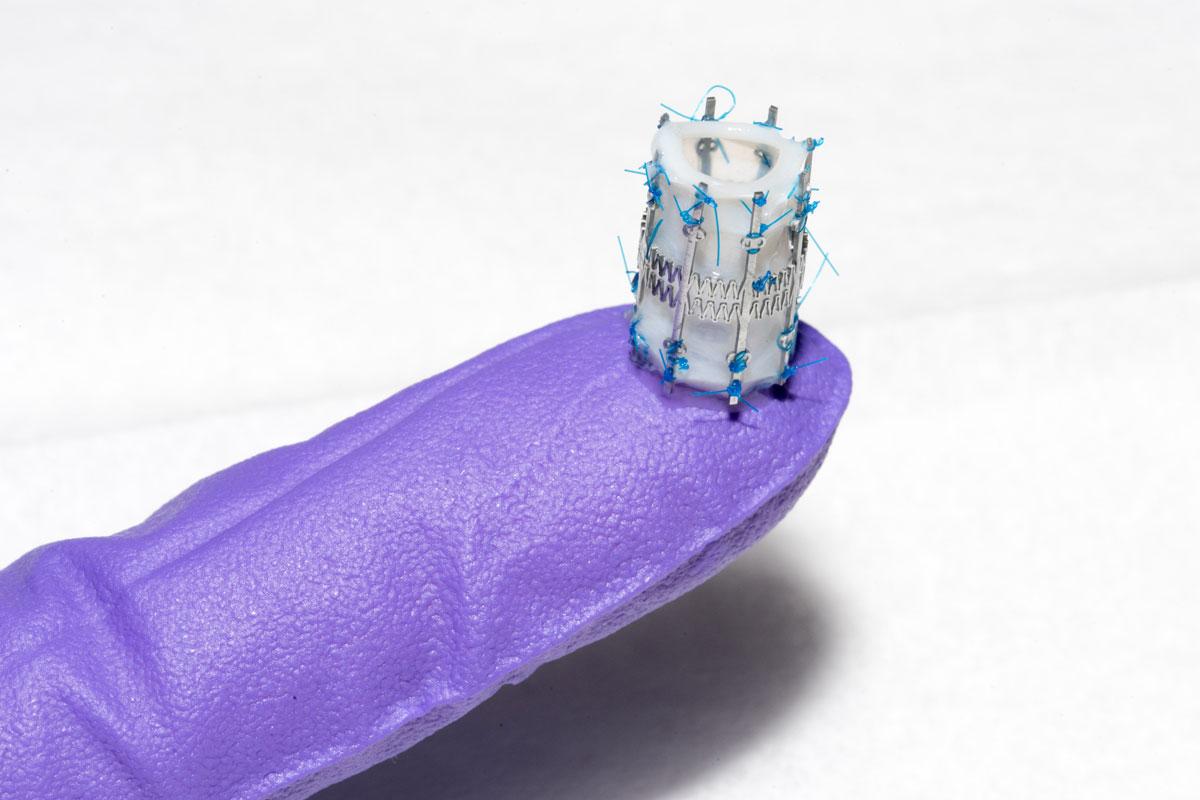
Figure 1: The LEAP Valve in a compressed state (Photo Provided)
The LEAP technology is focused on four separate components of device development: stent design, valve selection, stent-to-valve attachment, and surgical cuff design for implantation, which will allow the valve to adapt to the growing heart. The LEAP Valve will be implanted in a compressed state and will slowly expand using a low-force spring stent to adjust as the heart valve grows and widens.
Draper's heart valve stent has received awards from the American Society for Artificial Internal Organs3 and the Pediatric Device Innovation Symposium.4 In developing the device, Dr. Williams is working with pediatric clinicians at Boston Children's Hospital and Seattle Children's Hospital to conduct preclinical studies.
In addition to the LEAP technology, Dr. Williams and her team are addressing the major challenge of developing a new technology that will allow rapid attachment of the bioprosthetic tissue valve to the stent. The 'sutureless' alternative, known as MANTIS (Mechanical Adhesion to Tissue), relies on adhesive microstructures for mechanical integration. Current practices require suturing by hand, which is both time-consuming and expensive when trying to construct smaller devices. MANTIS will allow faster and less labor-intensive device manufacturing.
The LEAP Valve device is currently undergoing functionality testing to determine its performance under conditions that mimic the heart of a child from infancy to age five. Dr. Williams has filed a provisional patent and anticipates a forthcoming publication characterizing the preclinical animal model. The LEAP Valve is currently being tested in the model that span weight ranges similar to those of human infants and young children.
The information and data collected from this testing will meet the requirements for an Investigational Device Exemption submission to the U.S. Food and Drug Administration for First-In-Human Early Feasibility Studies. Soon after the project is completed, it is anticipated that infants and young children with the greatest need for valve replacement will be able to receive a LEAP Valve. In addition, the MANTIS technology may prove useful for hemorrhage control applications for treating Warfighters on the battlefield.
The innovative device and techniques being developed with this award are focused on the lives of the youngest military beneficiaries.
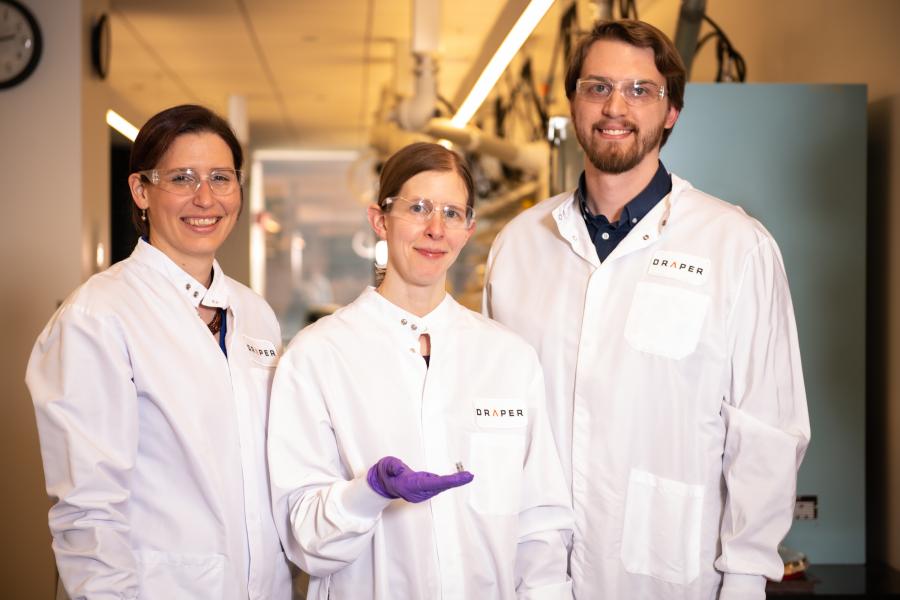
Draper Team: Dr. Corin Williams, center, holds a Leap Valve with members of the Draper Team, Dr. Stephanie Golman, left, and Mr. Daniel King, right, at the Charles Stark Draper Laboratory, Inc. in Cambridge, Massachusetts. (Photo Provided)
References:
1Data and Statistics on Congenital Heart Defects. Centers for Disease Control and Prevention. https://www.cdc.gov/heart-defects/data/index.html.
2Congenital Heart Defects in Children. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/congenital-heart-defects-children/symptoms-causes/syc-20350074.
3ASAIO Medical Device Entrepreneurs Forum. 2021. https://asaio.org/Conference/Awards/medical.cgi.
4The Pediatric Device Innovation Consortium. https://www.thepdic.org/projects.
Last updated Friday, December 19, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
