- Adoptive Cellular Therapy Targets Recurrent Pediatric Brain Cancer
- A Phase I Assessment of Mesenchymal Stem Cells for the Treatment of Multiple Sclerosis
- Novel Therapy Targeting Nerve Agent-Induced Seizures
- Photoacoustic Imaging of Epilepsy
- Web-based Visual Field Assessment and Diagnosis
- Optogenetic Control of Epileptic Seizures
- Sleep Loss and Metabolic Vulnerability
- Treatment of PTSD-Related Anger
- Tea Consumption Effects on Smoking-Related Oxidative Stress
- Studying Nerve Agent Exposure
- Neurologist and Breast Cancer Researchers Team-up to Unravel the Mysteries of Epileptogenesis
- Identification of Genes in Kidney Cancer Oncogenesis
- Corneal Protection for Burn Patients
- SNO and Pulmonary Arterial Hypertension
2011
Adoptive Cellular Therapy Targets Recurrent Pediatric Brain Cancer
Posted December 13, 2011
Duane Mitchell, M.D., Ph.D., Duke University Medical Center
Clinical Trial Award
Malignant brain tumors are a frequent cause of cancer death in children. Despite aggressive multi-modality therapy, which can be highly toxic, a significant number of children diagnosed with the most common malignant brain tumors will die from recurrence. Furthermore, survivors may experience severe, lifelong side effects that diminish their learning ability and motor functions. Thus, there is an urgent need for more effective and specific therapies that will improve the clinical outcomes for children affected by malignant brain tumors. Clinical outcomes observed in immunotherapy trials, using vaccines that target tumor-specific antigens expressed within brain tumors, have been very promising in adult patients. However, efforts to design pediatric brain cancer vaccines have been relatively inadequate, in part because of the limited availability of tumor tissue for cancer vaccine preparation. Dr. Duane Mitchell’s research team has developed a technique for making suitable cancer vaccines from as few as 100 tumor cells, which can be removed from small amounts of tumor tissue obtained during surgery or from a biopsy.
Dr. Mitchell received a Fiscal Year 2009 Clinical Trial Award from the Peer Reviewed Medical Research Program to conduct a single arm, prospective Phase I/II clinical trial in pediatric patients with medulloblastoma and primitive neuroectodermal tumors (MB/PNETs) to assess the toxicity and potential efficacy of an autologous dendritic cell (DC) vaccine following high-dose chemotherapy coupled with peripheral blood stem cell transplantation (PBSCT). DCs are one type of cell involved in regulating the T cell immune response to tumor cells. The primary objective of the proposed Phase I trial is to assess the safety and dose-limiting toxicity of the therapy; the primary objective of the Phase II trial is to estimate the progression-free survival rate of treated individuals.
The autologous vaccine will be constructed of DCs loaded with RNA isolated from the MB/PNETs. These RNA-loaded DCs will activate the immune system to recognize the differences between normal brain tissue and the malignant brain tumor cells. This would enable recognition and targeting of tumor cells for a potent immunologic response and a decrease in tumor size. Briefly, T cells will be harvested from the patient’s blood and activated in vitro with their own tumor-specific RNA-loaded DCs. The T cell population will then be expanded ex vivo (outside the body) to large numbers and returned to the patient after completion of chemotherapy treatments and PBSCT. These activated T cells will be restored to the patient after chemotherapy and transplantation to allow the body to recover normal white blood cell counts, which will help the tumor-specific T cells grow and establish a population in the patient. The ultimate goal is to improve the patient’s own ability to fight cancer through this new population of anti-MB/PNET T cells.Link:
A Phase I Assessment of Mesenchymal Stem Cells for the Treatment of Multiple Sclerosis
Posted December 13, 2011
Jeffrey Cohen, M.D., Cleveland Clinic Foundation
Multiple sclerosis (MS) is frequently a disabling neurodegenerative disease for which there is still no cure, although there are available treatments that are somewhat effective in delaying the progression of the disease. MS is characterized by two destructive processes: (1) Inflammation, which occurs early in the disease process and is less evident in the later stages and (2) Neurodegeneration, which occurs early in the disease process and continues as the disease progresses. This implies that to be effective, therapeutic strategies need to address multiple pathogenic mechanisms. Mesenchymal stem cells (MSCs), pluripotent cells in the bone marrow that do not develop into blood cells, may be beneficial in treating MS since they have immunologic effects as well as the ability to promote tissue repair. In vitro studies show that MSCs are able to differentiate into neuron-like cells, encourage other immature cells to become neuron-like, and decrease the activity of specific types of immune cells that are overactive in MS. Due to these properties, MSC transplantation has been considered as a mechanism to reduce immune-mediated damage and increase neural repair in MS.
Dr. Cohen received a Fiscal Year 2009 Peer Reviewed Medical Research Program Clinical Trial Award to conduct an open label Phase I study to evaluate the feasibility, safety, and tolerability of a single autologous MSC transplantation in 24 patients, ages 18-55, with relapsing forms of MS that have moderate to severe disability but are still able to walk. Bone marrow will be removed from the participant’s hip, MSCs will be purified, cultured/grown ex vivo until a sufficient cell number is achieved and re-infused intravenously to the participant (termed autologous transplantation). The safety and tolerability of the procedure will be determined by close monitoring of the participants for 6 months after MSC administration, including physical exams, blood work, and brain magnetic resonance imaging (MRI) scans.
To evaluate the results of MSC transplantation on MS disease activity and severity, the participants will be monitored by neurologic exam, vision testing, brain MRI, and optical coherence tomography prior to and for 6 months after MSC administration. If this study demonstrates that autologous MSC transplantation is safe in MS patients, further studies will be developed to more definitively assess the efficacy of MSC transplantation in MS.Link:
Novel Therapy Targeting Nerve Agent-Induced Seizures
Posted November 29, 2011
Jaideep Kapur, M.D., Ph.D., University of Virginia, Charlottesville, Virginia
Exposure to organophosphorous (OP) nerve gas agents can cause respiratory and gastrointestinal issues, seizures, coma, and even death. OP has been shown to cause these effects through inhibition of acetylcholinesterase, an enzyme necessary for the breakdown of the neurotransmitter acetylcholine, which functions normally to stimulate muscle contraction. Drugs such as atropine and 2-paraldoxime can restore the activity of acetylcholinesterase and reverse the peripheral damage if administered immediately after exposure. However, these drugs are not effective against the central action of nerve gas, seizures. Clinical studies using diazepam, the only compound approved by the U.S. Food and Drug Administration for treating nerve gas-induced seizures, showed that it did not provide complete protection. As a result, scientists have been testing other pathways that might be involved in nerve agent exposure seizures, such as the ion channel pathways. Ion channels are a diverse group of pore-forming proteins that regulate the flow of ions across the membrane in all cells. Recent studies have shown that function impairment of the M ion channels has similar effects as those of nerve agents, leading to frequent seizures and epilepsy, and that flupirtine, a drug that "opens" the M channel, prevents these effects.
Dr. Kapur received a Fiscal Year 2009 Peer Reviewed Medical Research Program Investigator-Initiated Research Award to test whether use of M type potassium channel modulators will effectively treat nerve agent-induced seizure. Dr. Kapur is testing the hypothesis that nerve agents exert their effect via inhibition of the M channel and use of drugs that open M channels will prevent the seizures.
Utilizing a previously developed OP-induced seizure animal model, Dr. Kapur demonstrated that M channels regulate glutamate release from presynaptic terminals. Moreover, he showed that diazepam and the M-channel activator, flupirtine, had a synergistic inhibitor effect on OP-induced frequent seizures. Although the mechanism of action and therapeutic efficacy of drugs are still under investigation, these promising data already suggest that targeting M channels could be promising in controlling nerve gas-induced seizures.Link:
Public and Technical Abstracts: M Current-Based Therapies for Nerve Agent Seizures
Photoacoustic Imaging of Epilepsy
Posted November 16, 2011
Huabei Jiang, Ph.D., University of Florida, Gainesville, Florida
Epilepsy is a brain disorder that involves repeated and spontaneous seizures caused by electrical disturbances, which in some cases originate from a defined brain region (seizure foci) and then are propagated to other parts of the brain. Treatment for epilepsy may involve surgery or medication. Many people with epilepsy can become seizure-free by using anti-epileptic drugs; however, approximately 25% of the drug-treated individuals do not respond to medication, and surgically removing the abnormal area of the brain where the seizures are originating may be the only treatment for them. Since the success of surgical treatment depends on the precise localization of the seizure foci, a number of imaging technologies, such as magnetic resonance imaging (MRI) and computed tomography (CT), have been employed to guide the surgical procedure. However, these approaches have several limitations, including insufficient temporal resolution, inability to monitor the patient for duration of time, and in some cases a requirement for invasive techniques.
Dr. Jiang received a Fiscal Year 2008 Advanced Technology/Therapeutic Development Award through the Peer Reviewed Medical Research Program to advance the ability to localize the seizure foci. Dr. Jiang will use photoacoustic tomography (PAT), a non-invasive imaging technique that combines the benefits of the high contrast of the optical imaging and the high resolution of the ultrasound imaging into a single modality to identify the seizure foci. Dr. Jiang hypothesizes that PAT offers the possibility to noninvasively track dynamical changes during seizure occurrence and plans to develop and evaluate the PAT system for epilepsy to noninvasively monitor in "real-time" changes that occur during seizure. "Real-time" visualization and analysis of the seizure events will increase the accuracy in identifying the seizure onset location, which will enhance the likelihood of successful surgical outcome.
At present, Dr. Jiang has successfully constructed, calibrated, and tested the PAT system using a number of extensive phantom experiments that simulate detection of seizure focus. Additionally, Dr. Jiang built an animal interface and demonstrated feasibility of in vivo imaging of rat brain. This improved photoacoustic imaging system showed the potential to provide three-dimensional and quantitative imaging of the rat brain for accurate epileptic seizure localization.
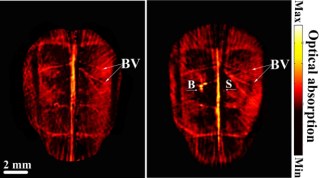
Dr. Jiang plans to further evaluate the PAT imaging system in rat epilepsy models; he plans to perform simultaneously PAT tomography and electroencephalography to these animals to monitor seizure activity continuously to characterize changes during seizures.Left: PAT of a normal rat brain. Right: Seizure focus detected by PAT (indicated by "B"). BV: blood vessels. B: Seizure focus chemically induced. S: injection of saline.
Link:
Public and Technical Abstracts: Photoacoustic Imaging of Epilepsy
Web-based Visual Field Assessment and Diagnosis
Posted August 4, 2011
Wolfgang Fink, Ph.D., California Institute of Technology, Pasadena, California
Vision is the primary sense used by most people in daily life. A variety of diseases or conditions, such as glaucoma and macular degeneration, if undetected, left untreated, or detected too late may lead to irreversible visual field loss and eventual blindness. As critical as having an unrestricted visual field is to most people, it is essential for those individuals involved in military operations in theater. In addition to diseases and disorders that may cause visual field loss, trauma, either ocular or to the brain, may also cause critical visual impairments.
There are a number of different ways currently used to assess the visual field of individual eyes. Whether it is manually by a clinician, through the use of visual field mapping tools such as the Amsler grid, or by other automated systems that map and calculate the visual field, these methods require fixating the examined eye straight forward and evaluating the extent of peripheral vision. However, most of the currently available automated visual field assessment equipment has limited sensitivity. In addition, these machines are bulky and not portable, limiting their use in geographically remote areas and/or military operational settings. Previously, Dr. Fink and his colleagues developed a technology that utilizes touch-sensitive display technology, called three-dimensional computer-automated threshold Amsler grid (3D-CTAG), with an increased sensitivity of visual field assessment and an improved ability to identify visual field defects that are often difficult to discern with traditional testing methods. Using the 3D-CTAG is fast and easy; the data necessary to make a diagnosis is obtained through non-invasive means and is of high spatial accuracy. In addition, the 3D-CTAG has been successfully evaluated in clinical studies to comprehensively test the visual field of individuals with conditions such as glaucoma, ocular hypertension, age-related macular degeneration, and optic neuritis. However, data obtained through the 3D-CTAG must be manually analyzed and interpreted before the clinician can make a diagnosis. One more drawback for remote settings is that clinical expertise may not be readily available to analyze and interpret these data. In military operational settings, a clinician may not be available to make necessary split-second decisions; in such situations, accurate automated data analysis would be beneficial.
Dr. Fink received a Fiscal Year 2008 Peer Reviewed Medical Research Program Advanced Technology/Therapeutic Development Award to use his previously developed 3D-CTAG technology as a starting point and to develop an advanced web-based system that will not only test the visual field, but will rapidly analyze, characterize, store, and share the test data to aid in the diagnosis of visual field defects.
The newly developed advanced system incorporates the 3D-CTAG, touch-screen technology, integrated analyses capabilities, and a database to assess visual performance and to analyze, interpret, and store the visual field data. To accurately analyze the 3D-CTAG-generated visual field data, Dr. Fink and his colleagues devised, implemented, and integrated a suite of numerical methods that (1) remove unwanted artifacts present in the 3D-CTAG raw data, (2) assess the visual field as a whole (i.e., visual field data transforms), and (3) characterize individual scotomas, i.e., visual field defects, within the examined visual field (i.e., scotoma data transforms).
This advanced visual field test and diagnosis system is easy to use. First, the system is calibrated by the user before assessing an individual's visual field. After calibration, the subject is kept fixed in position with a head-chin rest, with the non-test eye covered, in front of a touch-sensitive computer screen displaying an Amsler grid at a particular contrast. The subject traces on the screen with a finger the areas of the Amsler grid that are missing from the field of vision of the test eye. This procedure is repeated for varying contrast levels of the Amsler grid. Results are recorded in a database, processed, and analyzed. Following each eye's assessment, a graphical representation of the entire tested visual field, illustrating the location, extent, grade, and shape of existing visual field defects within, is automatically generated and displayed on the screen along with other critical data analysis information in alphanumerical form. A major benefit of this advanced system is that visual field defects may be assessed in the absence of a clinical expert: a significant advantage for individuals in remote areas and a critical advantage for individuals in military operational settings where it might allow for the timely application of counter measures to ensure the health and safety of personnel. Moreover, this system might assist a clinician's assessment through corroborating or contradicting a diagnosis. The next steps for Dr. Fink and his team are to further refine the system and to continue to evaluate its performance in clinical studies.
Dr. Fink's advanced visual field test and diagnosis system offers a new perspective for evaluating visual fields that includes computer-assisted diagnosis and telemedicine opportunities for individuals in geographically remote areas and/or military operational settings.
Link:
Optogenetic Control of Epileptic Seizures
Posted July 26, 2011
Anna Majewska, Ph.D., University of Rochester, Rochester, New York
Sydney Cash, M.D., Massachusetts General Hospital, Boston, Massachusetts
Brain cells continuously generate tiny electrical impulses that travel along a network of nerve cells in the brain and throughout the whole body. Brain function is normally controlled by a balance between excitatory and inhibitory networks; problems occur when these opposing networks are out of balance. Epilepsy is a brain disorder involving repeated and spontaneous seizures caused by inappropriately excited electrical signals in the brain. This unusual level of excitatory signals is the result of an imbalance between the excitatory neuron activity, which drives epileptic activity, and inhibitory neuron activity, which reduces it. Epilepsy is currently treated by medications, surgery, and/or electrical stimulation. However, none of these therapeutic options is able to target specific neurons only during seizure episodes; consequently, they also affect seizure-free brain activity and, as such, have potential side effects. Therefore, new treatment alternatives that expressly control the activity of specific circuits only during seizures, without affecting normal brain function, are very desirable. Recent advances in the use of genetics for optical control of neuronal activity make it possible to develop, novel methods for controlling and studying epileptic seizures.
Dr. Majewska and Dr. Cash received Fiscal Year 2008 Translational Research Awards through the Peer Reviewed Medical Research Program to test a new approach for treating seizures that will potentially overcome the limitations and side effects of current treatment options. These partnering Principal Investigators (PIs) plan to combine optical and genetic approaches (optogenetics), in a rodent model, to alter the electrical activity of specific neurons during epileptic episodes using light activation. The overall goal of this study is to develop a process that will deliver light stimulation in epileptic areas at the start of a seizure to inhibit excitatory cell activity and/or increase inhibitory cell activity. Their hypothesis is that the targeted effects of light on specific circuit elements will quickly prevent the seizure from spreading. Importantly, patients using this treatment option should not suffer side effects during seizure-free periods of everyday life.
Membrane-bound light-sensitive proteins, called opsins, have the ability to inhibit or enhance the electrical activity of nerve cells when they are illuminated. Drs. Majewska and Cash are genetically altering selected neurons to express specific opsins using in vitro and in vivo animal experiments. The hope is that the activity of these opsin-expressing cells will be positively affected in response to light stimulation during seizure episodes, but that neuron function will not be affected when seizures are not occurring. Excitatory neurons will be altered to express inhibitory opsins, while inhibitory neurons will be altered to express excitatory opsins using safe gene therapy approaches. A light source will also be implanted at the same time to illuminate areas of the brain where seizures are initiated. An electrophysiological monitor will be used to record brain activity. Abnormal activity patterns in the brain that precede seizures or indicate the start of an epileptic event will trigger a circuit that will flood the targeted brain area with light and shut down excitatory activity while enhancing inhibitory neural activity, preventing both the initiation and spread of the seizure. The individual receiving treatment may not even know that an epileptic episode has just been avoided.
Preliminary data from simultaneous injection of opsins, and implantation of a light source and an electrophysiological monitor recording in rat hippocampus showed that seizure activity can be delayed using light activation of specific hippocampal neuronal populations. The PIs are currently optimizing the timing of the flood of light in the brain with regard to seizure start and are developing automatic seizure detection software. This optogenic approach is not only a promising new therapeutic approach to treating epilepsy, but it may also prove useful for treating other chronic neurological diseases.
Link:
Public and Technical Abstracts: Optogenetic Control of Seizures
Sleep Loss and Metabolic Vulnerability
Posted July 21, 2011
Eve Van Cauter, Ph.D., University of Chicago, Chicago, Illinois
While obesity and diabetes epidemics continue to grow, some researchers believe that the high prevalence of chronic partial sleep loss in contemporary society has contributed to this disturbing trend. There is strong evidence that large differences in both metabolic and cognitive vulnerability can be attributed to sleep loss. Recent studies suggest variability in diabetes risk associated with sleep loss may correlate with slow-wave activity (SWA), or low frequency brain waves that are measurable during slow-wave sleep periods. It is believed that individuals with low SWA are at greater risk for developing diabetes after chronic partial sleep loss than those individuals with higher SWA. Dr. Eve Van Cauter received a Fiscal Year 2006 Investigator-Initiated Award through the Peer Reviewed Medical Research Program to study whether SWA can be used as a predictor of metabolic vulnerability to sleep loss in a subject population with gender, ethnic, and age distributions.
Dr. Van Cauter and her research team determined the correlation of sex, body mass index (BMI), ethnicity, and age with SWA levels across 128 electroencephalogram (EEG) recordings. (An EEG is a test that measures and records the brain's electrical activity such as SWA.) The baseline levels of SWA in the sleep EEG of volunteers who slept 8-9 hours each night over two nights demonstrated that women have higher SWA than men and demonstrated that overall, increased age was associated with reduced SWA levels. Interestingly, BMI did not correlate with the SWA levels. Studies of the differences in SWA levels between ethnic groups showed that after adjusting for age and sex, African Americans and Hispanics, known to be at a higher risk of type 2 diabetes compared to whites and Asians, had a lower SWA than whites and Asians. More studies in this area will help determine whether there is a correlation between ethnic risk for diabetes and SWA levels. With regard to age, the data demonstrated that between the ages of 21 and 30, there are large inter-individual variations in SWA that are only partially predicted by sex and ethnicity. This may be a critical age range to examine the impact of individual differences in SWA; it is an age range that includes nearly 50% of active duty Army personnel.
Additionally, Dr. Van Cauter's team is currently examining diabetes risk in ongoing sleep deprivation research where sleep EEG and glucose levels are being monitored. Preliminary data from this study indicate a clear and progressive decrease in global vigor and increase in appetite during recurrent sleep deprivation. Moreover, sleep deprivation resulted in an increase in glucose levels, despite a robust increase in insulin, and decreased insulin sensitivity. Through these ongoing studies, Dr. Van Cauter hopes to better understand the relationship between metabolic vulnerability and sleep loss, which might ultimately provide the basis for the identification of countermeasures to the deleterious effects of sleep loss on metabolism.
Publications:
Spiegel K, Tasali E, Leproult R, and Van Cauter E. 2009. Sleep loss and sleep disorders: Impact on hormones and metabolism. Nature Clinical Practice Endocrinology & Metabolism 5(5):253-261.
Spiegel K, Tasali E, Leproult R, and Van Cauter E. 2009. Effects of poor and short sleep on glucose metabolism and obesity risk. Nature Reviews Endocrinology 5(5):253-261.
Van Cauter E and Spiegel K. 2009. Sleep and diabesity. Obesity and Metabolism Journal 5:1.
Van Cauter E, Spiegel K, Tasali E, and Leproult R. 2008. Metabolic consequences of sleep and sleep loss. Sleep Medicine 9(1):S23-S28.
Van Cauter E and Knutson KL. 2008. Sleep and the epidemic of obesity in children and adults, 2008. European Journal of Endocrinology 159(1):S59-S66 (Epub 2008 Aug 21).
Link:
Public and Technical Abstracts: Individual Differences in Diabetes Risk: Role of Sleep Disturbances
Treatment of PTSD-Related Anger
Posted June 23, 2011
M. Tracie Shea, Ph.D., Brown University, Providence, Rhode Island
Posttraumatic stress disorder (PTSD) is one of the most common debilitating and chronic psychological disorders diagnosed among military service members deployed to hazardous locations. In addition, there is an established association between experiencing trauma and exhibiting anger with negative consequences. This association, for combat veterans especially, is one possible factor interfering with recovery from psychological trauma. Dr. Tracie Shea received a fiscal year 2004 Investigator-Initiated Research Award through the Department of Defense Peer Reviewed Medical Research Program to adapt a cognitive-behavioral intervention (CBI) for the prevention of negative consequences of PTSD-associated anger in military personnel returning from hazardous deployment arenas.
Dr. Shea adapted a CBI technique originally developed by Dr. Raymond Novaco, adding several key elements: A cognitive restructuring component for the identification and modification of beliefs and interpretations; behavioral coping strategies; and inoculation training, which uses exposure through imagery to anger-inducing scenes. Adaptations specific for returning military personnel were made to the content. A randomized pilot study was conducted to evaluate whether treatment with the modified CBI would result in less anger and aggression, less severe PTSD symptoms, and better overall functioning and quality of life. Dr. Shea compared the outcome of the modified CBI to that of a supportive intervention (SI), which served as the control group. The SI employs problem-solving skills to address current stressors and concerns, along with education on common reactions to trauma and typical stressors. Study participants were military personnel, recently returned from a war zone deployment, who had been exposed to trauma. Each subject also exhibited at least two symptoms (one being anger/irritability) of hyperarousal associated with at least moderate impairment. Primary outcome measures assessed (1) expression and control of anger and (2) severity, type, and frequency of aggressive behavior. Secondary outcome measures included functional status and PTSD symptoms. Outcome measures were recorded prior to treatment initiation, at treatment termination, and three months following termination of treatment.
A comparison between pre- and post-treatment outcomes showed that Dr. Shea's modified CBI resulted in significant improvement on multiple anger outcome measures when compared to the SI control. The CBI group also demonstrated significant improvement in functioning, suggesting that the effects of this treatment extended beyond the target (anger) alone. These improvements were largely maintained over three months of follow-up. However, despite the improvement in anger and some areas of functioning, the CBI did not appear to abate other symptoms of PTSD.
These preliminary, pilot study data are exciting and illustrate the need for additional studies, using a larger number of human subjects, to confirm the efficacy of this modified CBI protocol. A compelling question that Dr. Shea plans to ask is whether fewer sessions of CBI might be effective. Future studies also need to include more women and minorities, to determine if sex or race plays a role in response to this potential new anger management therapy.
Link:
Technical Abstract: Treatment of PTSD-Related Anger in Troops Returning From Hazardous Deployments
Tea Consumption Effects on Smoking-Related Oxidative Stress
Posted May 19, 2011
Iman Hakim, M.D., Ph.D., MPH, University of Arizona, Tucson, Arizona Investigator-Initiated Research
Some research findings have associated a decreased occurrence of cancer in people who regularly drink tea. This may be associated with the strong antioxidant effect of polyphenols found in tea. Antioxidants, such as polyphenols, are molecules that may prevent or slow oxidative damage caused by reactive oxygen species (ROS) resulting from the body's use of oxygen. ROS not bound by antioxidants may play an important role in the initiation and progression of a variety of diseases including cancer. Cigarette smoke or oxidants formed in the lungs of smokers contain numerous ROS-generating compounds that can damage DNA directly or indirectly, and may also trigger oxidative damage to cellular components, including lipids contributing to the development of cancer and other respiratory diseases.
Dr. Iman Hakim received a fiscal year 2002 Investigator-Initiated Research Award from the Department of Defense Peer Reviewed Medical Research Program to conduct a randomized, placebo-controlled, double-blinded, three-arm clinical trial aimed at identifying the effects of high tea consumption on biological markers of oxidative stress related to smoking. These biological markers included: (1) the DNA damage biomarker 8-hydroxydeoxyguanosine (8-OHdG) found in urine and (2) the lipid damage biomarker 8-F2-isopranes (8-epi-PGF2) found in urine. One hundred fifty-four participants (71 male and 83 female) were stratified by smoking status [current or former smokers of 25 or more packs per year (1.3-3.8 cigarettes a day)] and sex, and who drank green tea, black tea, or placebo for 6 months.
Study results obtained by Dr. Hakim and her research team show that specific cohorts in this study responded to tea consumption as evidenced by decreased levels of oxidative stress biomarkers. Among the green tea consumers, female current smokers benefitted most and showed a 35% significant decrease in DNA damage; no effect was observed in female former smokers, or male smokers, both current and former. While black tea consumption had mixed results overall, former smokers appeared to benefit the most from drinking it. Male former smokers consuming black tea had a 37% decrease in DNA damage and female former smokers consuming black tea showed a significant (35%) decrease in lipid damage. These data suggest that drinking tea, whether green or black, may potentially modulate tobacco-related DNA and/or lipid oxidative damages especially among females.
Link:
Studying Nerve Agent Exposure
Posted May 3, 2011
Oksana Lockridge, Ph.D., University of Nebraska Medical Center
Exposure to organophosphorus nerve agents (OP) is potentially fatal due to asphyxiation, as control is lost over respiratory muscles. Symptoms of OP exposure may include contraction of pupils, tightness in the chest, excessive secretions, gastrointestinal pain, and convulsions; death can occur by asphyxiation with loss of control over respiratory muscles. OP causes these effects through inhibition of acetylcholinesterase, an enzyme necessary for the breakdown of the neurotransmitter acetylcholine, which functions normally to stimulate muscle contraction. Studies have shown that OP binds covalently (permanently) to the amino acid serine on the acetylcholinesterase active site where the breakdown of the acetylcholine takes place, which leads to acetylcholine accumulation and constant muscle contraction. There is evidence that some people suffer chronic illness from a dose of OP too low to inhibit acetylcholinesterase, which may indicate that OP-reactive proteins exist that are more sensitive to OP exposure than acetylcholinesterase. Dr. Lockridge received a 2006 Investigator-Initiated Award through the Department of Defense Peer Reviewed Medical Research Program to identify new protein targets (i.e., biomarkers of exposure) that are modified by exposure to OP and new bioscavengers for protection against nerve agent toxicity.
Using mass spectrometry, an analytical method used to determine molecular mass, composition, and structure, Dr. Lockridge identified new binding motifs for OP in proteins that have no serine active site. She and her research team showed that OP binds to the amino acid tyrosine on plasma albumin. Contrary to OP-serine bonds that decay quickly, these data demonstrated that the OP-tyrosine bond is stable and irreversible, suggesting that OP exposure could be monitored by analyzing OP-tyrosine adducts in blood samples taken weeks after the exposure incident.
Further analyses of blood samples from human subjects exposed to pesticides showed that OP bound to tyrosine 411 of albumin, identifying albumin as a new biomarker for OP exposure. This suggests that antibodies could be developed that recognize OP-tyrosine adducts on proteins in plasma leading to detection of OP exposure. In addition to albumin, Dr. Lockridge showed that OP binds covalently to the amino acid tyrosine in tubulin. Mice treated with low doses of OP that do not inhibit acetylcholinesterase had thin microtubules, few associated proteins, and OP-modified tubulin in their brains as it was detected by nanoimaging. Taken together, these observations indicate that cholinesterases are not the only clinically relevant targets for OP. This lays the groundwork for understanding the neurotoxicity mechanism by low-dose exposure and opens a pipeline for the development for new diagnostics.
In addition to acetylcholinesterase, OP permanently binds to the amino acid serine in plasma, butyrylcholinesterase (BChE), and inhibits its enzymatic activity. Loss of BChE activity is considered a biomarker of exposure to OP agents. Dr. Lockridge developed mass spectrometry methods to detect OP adducts on the active site serine of human BChE. Using these methods, she was able to detect OP agent adducts on BChE in plasma of exposed human subjects.
While the OP binding to BChE causes inhibition of BChE enzymatic activity, it also inactivates the OP and renders it harmless. The irreversible binding and inactivating function of BChE against a broad spectrum of OP poisons is an attractive feature for its use as a prophylactic agent to prevent incapacitation and death by chemical warfare using OP nerve agents. This potential has led to extensive research efforts in recent years devoted to producing large quantities of human BChE. In the course of her work, Dr. Lockridge determined how to optimize the production of the stable tetrameric BChE in cell culture. This tetrameric form of BChE, made up of four combined molecules and common in nature, has a half-life of 11-14 days, compared to the monomer half-life of 20 minutes, and therefore may be the best form of BChE preventive treatment against chemical exposure.
Most recently, Dr. Lockridge and her collaborators successfully utilized a mouse model to test the feasibility of using adenovirus to deliver clinically relevant amounts of BChE to prevent toxicity caused by exposure to nerve agents. These exciting results may one day lead to the development of a functional and practical prophylactic for the effects of exposure to OP.
Publications:
Li H, Tong L, Schopfer LM, Masson P, and Lockridge O. 2008. Fast affinity purification coupled with mass spectrometry for identifying organophosphate labeled plasma butyrylcholinesterase. Chemico-Biological Interactions 175(1-3):68-72. PMID: 18586231.
Jiang W, Duysen EG, Hansen H, Shlyakhtenko L, Schopfer LM, and Lockridge O. 2010. Mice treated with chlorpyrifos or chlorpyrifos oxon have organophosphorylated tubulin in the brain and disrupted microtubule structures, suggesting a role for tubulin in neurotoxicity associated with exposure to organophosphorus agents. Toxicological Sciences 115(1):183-193. PMID: 20142434.
Li B, Ricordel I, Schopfer LM, Baud F, Mégarbane B, Nachon F, Masson P, and Lockridge O. 2010. Detection of adduct on tyrosine 411 of albumin in humans poisoned by dichlorvos. Toxicological Sciences 116(1):23-31. PMID: 20395308.
Links:
Technical and Public Abstracts: Mass Spectrometry to Identify New Biomarkers of Nerve Agent Exposure
Neurologist and Breast Cancer Researchers Team-up to Unravel the Mysteries of Epileptogenesis
Posted April 28, 2011
Audrey S. Yee, M.D., University of Colorado Denver, Aurora, Colorado
Amy S. Yee. Ph.D., Tufts University School of Medicine, Boston, Massachusetts
Epileptogenesis is the process by which a normal brain undergoes morphologic and biologic changes that ultimately result in the development of epilepsy. Changes in the brain include abnormal neuronal signaling patterns and changes in synaptic plasticity. While the various stages of epileptogenesis are not well defined, epileptogenic stimuli may include various events such as prolonged seizure called status epilepticus (SE), brain injury, or infection as the initiating incident. Epileptogenesis, during which no obvious symptoms of seizures occur, may begin within weeks to years after the initial insult. After this latent period, changes in the brain result in epilepsy, a brain disorder which causes recurring seizures. Interestingly, intracellular signaling through the Wnt pathway, known to be misregulated in cancer cells, also plays an important role in neurodegenerative conditions and synaptic plasticity. Yet, the role of Wnt signaling during epileptogenesis has not been examined.
Combining their seemingly disparate interests, Dr. Audrey Yee, a neurologist who studies the basic mechanisms of anticonvulsants and the cellular mechanisms of epilepsy, and Dr. Amy Yee, a breast cancer researcher who studies the molecular mechanisms of tumor suppression, decided to pursue obtaining quantitative data regarding alterations in Wnt signaling during the early epileptogenic event SE. Funded by a Fiscal Year 2009 Investigator-Initiated Research Award through the Peer Reviewed Medical Research Program, these partnering Principal Investigators (and first cousins) collaborate to utilize their multidisciplinary research interests to find new targets to treat early stages of epileptogenesis. Using a whole animal model of epilepsy, they plan to test three hypotheses: (1) Wnt signaling is altered following induction of SE; (2) Wnt signaling modulates early events in epilepsy; and (3) modulation of Wnt signaling after induction of SE could have therapeutic efficacy. Ultimately, their goal is to identify potential early interventions following SE that might prevent its downstream effects and prevent the epileptogenic process.Links:
Technical and Public Abstracts: Epilepsy and the Wnt Signaling Pathway
Identification of Genes in Kidney Cancer Oncogenesis
Posted March 24, 2011
Maria Czyzyk-Krzeska, M.D., Ph.D., University of Cincinnati, Cincinnati, OH
Renal clear cell carcinoma (RCC) is a frequent malignant cancer. Its incidence is specifically high for military members after the 4th decade of life. Currently existing therapies have a limited impact on survival in the case of metastatic disease, increasing the median overall survival by only 1.5 to 6 months, with a very limited number of long-term survivors. Thus, the studies of molecular mechanisms involved in RCC leading to the discoveries of new treatments are of crucial importance.
The loss of activity of the major tumor suppressor von Hippel-Lindau protein (pVHL) is an early and frequent event in the development of RCC. The laboratory of Dr. Maria Czyzyk-Krzeska at the University of Cincinnati is engaged in investigating different tumor suppressing and oncogenic pathways regulated by VHL in RCC. This work, supported by Investigator-Initiated Research Award from the Fiscal Year 2006 Peer Reviewed Medical Research Program (PR064135), led to the discovery of two novel regulatory pathways that may be used in the future for the development of new treatment options for RCC.
First, Dr. Czyzyk-Krzeska's laboratory discovered that the large subunit of RNA Polymerase II, a protein involved with gene transcription, is regulated by pVHL, a potential mechanism by which VHL coordinates gene transcription. The laboratory has shown that that pVHL binds to the subunit Rpb1 of RNA polymerase II and regulates its activity. This binding requires hydroxylation of specific proline within Rpb1 by prolyl hydroxylase, PHD1. Moreover there is an increased PHD1-mediated hydroxylation and pro-tumorigenic activity of Rpb1 in human renal cancer tumors as compared to normal kidney cells. Thus, proline hydroxylation of Rpb1 and the activity of PHD1 represent potential new drug targets for RCC treatments.
Second, the Dr. Czyzyk-Krzeska and her colleagues discovered another novel pathway in RCC. It was observed that expression of a small non-coding RNA (microRNA 204) was positively regulated by VHL, and was lost in human RCC tumors corresponding to cancer progression. This microRNA has tumor suppressing activity and is cytotoxic to renal cancer cells. An important activity of the microRNA-204 is inhibition of macroautophagy, a process by which cells obtain nutrients from intracellular sources at the time of extracellular deprivation of nutrients. Importantly, macroautophagy is necessary for tumor growth and cancer progression. Identification of this pathway lays ground for further development of novel therapeutic approaches for treatment of renal cancer.
Corneal Protection for Burn Patients
Posted February 10, 2011
Irene E. Kochevar, Ph.D., Massachusetts General Hospital, Boston, Massachusetts
Anthony J. Johnson, M.D., Brooke Army Medical Center, Fort Sam Houston, Texas
Many burn patients develop eye complications, such as infection or corneal ulceration, and possible loss of sight, even when their eyes are not directly damaged by the burn. Facial scarring during burn injury recovery may cause the skin to contract away from the eyes, forcing a patient's eyes to remain open day and night. This precludes blinking, which is needed to distribute tears over the cornea to keep them wet and healthy. When the cornea is dry for long periods, it becomes dehydrated, leading to loss of the epithelial layer; infection; corneal ulceration; and, eventually, loss of vision. Current methods for maintaining a hydrated cornea involve frequent addition of moisturizing drops or covering the cornea with a layer of amniotic membrane held in a ring, which acts like an epithelial layer to protect and moisturize the eye. The former method is very inefficient and the latter is very expensive because the amnion dissolves within two days and costs approximately $900 per eye/membrane. Drs. Irene E. Kochevar and Anthony J. Johnson, a Colonel in the U.S. Army, received a Fiscal Year 2008 Translational Research Award from the Peer Reviewed Medical Research Program to develop a tissue to cover the cornea of burn patients that will prevent eyes from drying out and will preserve the vision of patients that will be more efficient and cost effective.
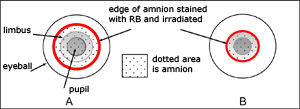
Drs. Kochevar and Johnson proposed to develop a more degradation-resistant amniotic membrane or "new bandage" to use with hydrogels and growth factors to keep the corneas of burn patients healthy during the period when they cannot close their eyes. Due to its anti-inflammatory and healing-promoting properties, these investigators and their research teams are using cryopreserved or freeze-dried human amniotic membrane as the basic tissue to cover the cornea due to its anti-inflammatory and healing-promoting properties. To decrease the degradation rate of the amnion, amniotic membrane proteins were crosslinked using several methods differing in their molecular mechanisms (photochemical, UV and enzymatic methods). Preliminary in vitro studies demonstrated that crosslinking proteins of the amniotic membranes resulted in 35% to 100% inhibition of amnion degradation. Methods of photobonding will be assessed as this may provide an additional alternative to suturing of amniotic membrane to cornea. Additionally, the PIs are devising ways to increase the ability of the amnion to hydrate the cornea by combining hydrogels and various growth factors with the amnion. This will also serve to reduce any inflammation on the ocular surface and increase associated healing factors. Final studies in an animal model will show proof-of-concept that a combination of crosslinking and addition of a hydrogel to human amnion will provide an effective layer on the cornea to allow for healing during facial burn rehabilitation. Dr. Kochevar and COL Johnson believe that, if these studies are successful, corneal damage resulting from extended drying during recovery from severe facial burns will be minimized, resulting in retention of vision. In addition, care for these patients' eyes will be simplified during their recovery, and the costs of treating their corneas will be greatly reduced.Links:
Public and Technical Abstracts: Corneal Protection for Burn Patients
SNO and Pulmonary Arterial Hypertension
Posted February 3, 2011
Lisa A. Palmer, Ph.D., University of Virginia, Charlottesville, Virginia
Pulmonary arterial hypertension (PAH) is characterized by increased pulmonary arterial pressure and structural changes in the lung vasculature, which, if not treated, can lead to the development of heart failure and death. Hypoxia (insufficient oxygen supply) is one of a variety of conditions and diseases associated with the development of PAH. A number of pathogenic pathways for hypoxia-induced PAH have been described including impaired S-nitrosothiol (SNO) signaling. In the pulmonary endothelium, SNO formation requires endothelial nitric oxide synthase (eNOS) whereas its breakdown involves S-nitrosoglutathione reductase (GSNO-R). Under healthy conditions, levels of SNO hemoglobin from the right ventricle of male and female mice are the same, suggesting that the activities of eNOS and GSNO-R are balanced. Notably, both proteins are regulated by sex steroids: eNOS activity is increased by estrogen and GSNO-R activity is decreased by testosterone. Dr. Lisa Palmer, a recipient of a fiscal year 2006 Investigator-Initiated Award from the Peer Reviewed Medical Research Program, is determining the role of the SNO signal transduction pathway and the sex hormones in the development of PAH.
Dr. Palmer and her research team introduced a new animal model of PAH, which mimics the chronic hypoxia vascular pathology through chronic N-acetylcysteine (NAC) administration to normoxic mice (mice with a sufficient oxygen supply). NAC-treated mice exhibit increased right ventricular pressure and hypertrophy and pulmonary vascular remodeling. In blood, NAC was converted to S-nitroso-N-acetylcysteine (SNOAC), which resulted in decreased SNO levels. The researchers demonstrated that SNOAC was necessary for the development of PAH in this model. Examination of gender differences in this mouse model of PAH showed that the lungs of female mice have greater GSNO-R activity than the lungs of male mice. Also, castration, which results in testosterone depletion, resulted in increased GSNO-R activity in the males to the level seen in females; increased GSNO-R activity is associated with blocked development of PAH. These results suggest that the sex-related differences in GSNO-R activity levels may play an important role in male susceptibility to and female protection from the development of PAH.Publication:
Palmer LA, Doctor A, Chhabra P, Sheram ML, Laubach VE, Karlinsky MZ, Forbes MS, Macdonald T, and Gaston B. 2007. S-nitrosothiols signal hypoxia-mimetic vascular pathology. The Journal of Clinical Investigation 117:(9) 2592-2601.
Links:
Public and Technical Abstracts: S-nitrosylation and the Development of Pulmonary Hypertension