Peer Reviewed Cancer



Posted May 8, 2020
Julien Fourcade, Ph.D., Pharm.D., University of Pittsburgh

Dr. Julien Fourcade
Over the last 30 years, melanoma cases have increased in the U.S., most likely related to increase sun exposure. According to the American Cancer Society, it is the fifth most common type of cancer in the United States, representing 5.3% of all new cancer diagnoses every year. Melanoma is of particular interest to the U.S. military because active duty Service members spend prolonged periods outside, especially during deployment. Amongst all military personnel, the greatest incidence rates are seen in the Air Force, Navy, and the Marines.
The last 10 years have seen multiple promising advancements in the treatment strategies for melanoma. Recently, much focus has been in the area of immunotherapy, a type of treatment that targets the immune system to help the body fight cancer. One type of immunotherapy, called checkpoint inhibitors, targets inhibitory molecules expressed on T cells. Checkpoint inhibitors allow T cells to become activated and kill tumor cells. The US Food and Drug Administration has approved several checkpoint inhibitors for the treatment of melanoma and other cancers. However, not every patient responds to the currently approved inhibitors, so there is a need to develop checkpoint inhibitors targeted toward other immune molecules.
Dr. Julien Fourcade, with a FY14 Career Development Award, proposed to identify novel mechanisms to activate the immune system to fight cancer. He focused on a type of immunosuppressive cells called regulatory T cells (Tregs). In many cancers, infiltration of Tregs into tumors are associated with a poor prognosis. Depleting Tregs is potentially one strategy to promote activation of the anti-tumor immune response. Dr. Fourcade showed that Tregs in the blood and within tumors of metastatic melanoma patients express high levels of an inhibitory molecule called TIGIT; these cells create a suppressive environment so that other immune cells cannot activate their anti-tumor functions. TIGIT competes for the same ligand (PVR) with another molecule called CD226. Activation of TIGIT with PVR further promotes Treg immunosuppressive functions. However, activating CD226 with PVR in combination with blocking anti-TIGIT antibodies shifts Tregs towards more stimulatory immune functions. Therefore, targeting these molecules may promote anti-tumor activity.
The second part of this project assessed whether Tregs could be depleted in patients by targeting TIGIT with antibodies to reverse Treg-induced immunosuppression. Dr. Fourcade demonstrated that Tregs can be depleted with targeted antibodies designed to recruit natural killer cells to kill Tregs. These findings provide a rationale for novel immunotherapies aimed at blocking TIGIT and activating CD226 in order to reverse the suppression of antitumor responses mediated by Tregs in patients with advanced melanoma. The development of new checkpoint inhibitors provides additional therapeutic options for patients who are not candidates for anti-PD1 or anti-CTLA4 treatment, therefore creating more opportunities to cure melanoma.
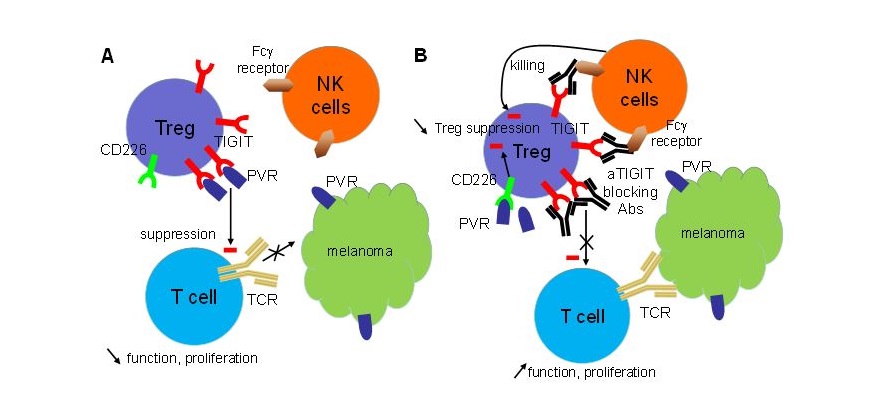
- PVR acts through the receptor TIGIT to enhance tumor-infiltrated Treg suppressive capacities, which in turn inhibits anti-tumor T cells in the tumor microenvironment and promote tumor progression.
- In the presence of anti-TIGIT antibodies (Abs), TIGIT on Tregs is blocked and PVR can act through CD226 to reduce Treg suppressive functions and proliferation, which in turn increases anti-tumor T cell functions and proliferation in the tumor microenvironment. NK cells bind to anti-TIGIT Abs on Tregs with their Fcϒ receptors, which induces the killing of TIGIT-expressing Tregs.
- PVR acts through the receptor TIGIT to enhance tumor-infiltrated Treg suppressive capacities, which in turn inhibits anti-tumor T cells in the tumor microenvironment and promote tumor progression.
- In the presence of anti-TIGIT antibodies (Abs), TIGIT on Tregs is blocked and PVR can act through CD226 to reduce Treg suppressive functions and proliferation, which in turn increases anti-tumor T cell functions and proliferation in the tumor microenvironment. NK cells bind to anti-TIGIT Abs on Tregs with their Fcϒ receptors, which induces the killing of TIGIT-expressing Tregs.
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
