Peer Reviewed Cancer



- Assessment of Melanoma-Specific Novel Markers in the U.S. Military Population
- Highlights of a Noninvasive Genetic Test for Colon Cancer Screening
Assessment of Melanoma-Specific Novel Markers in the U.S. Military Population
Posted May 5, 2011
Mohammed Kashani-Sabet, M.D., California Pacific Medical Center, San Francisco, California
Sancy Leachman, M.D., Ph.D., University of Utah, Salt Lake City, Utah
Although it remains one of the rarer types of skin cancer, melanoma is linked to about 75% of skin cancer-related deaths. Exposure to the sun or ultraviolet radiation (UVR) has been identified as one of the strongest environmental risk factors for melanoma development. In addition to sun/UVR exposure, genetic and molecular factors have been recognized as important components associated with the onset and progression of the disease. Since the accurate diagnosis of melanoma based on histopathological evaluation can be very challenging, the development of more sensitive and specific diagnostic tools is necessary.
Recipients of a Fiscal Year 2009 Collaborative Translational Science Award, Drs. Mohammed Kashani-Sabet and Sancy Leachman are proposing to examine a number of genetic markers of melanoma susceptibility, and to validate multi-marker diagnostic and prognostic assays for melanoma. The groundwork for this study is based on the identification of molecular markers that are differentially expressed at various stages of melanoma. With extensive expertise in the clinical care of melanoma patients, melanoma genetic epidemiology, cancer pathology, and progression markers, a group of talented clinicians and scientists have joined forces to assess known risk factors for melanoma among the active duty military population utilizing serum samples from the U.S. Military. Military personnel are extensively exposed to UVR as a result of their deployment assignments. Accurate assessment of risk and diagnostic factors for melanoma will help in identifying service men and women at higher risk of developing melanoma; this study may yield a simple melanoma risk assessment model that could be translated into the clinic. Additionally, the efficacy of melanoma-specific pre-selected multi-marker molecular diagnostic and prognostic assays, based on immunohistochemistry and quantitative polymerase chain reaction (PCR) platforms, will be validated within the U.S. Military population.
If successful, this study will benefit the melanoma community and the military population with clinically translatable molecular tools that can be used for the assessment of melanoma susceptibility, diagnosis, and prognosis.
Links:
Public and Technical Abstracts: Molecular Determinants of Melanoma Susceptibility and Progression
Highlights of a Noninvasive Genetic Test for Colon Cancer Screening
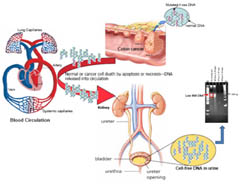
Dr. Su discusses her work on developing a non-invasive genetic urine test for colorectal cancer.
Posted March 10, 2011
Dr. Ying-Hsiu Su, Drexel University
Colorectal cancer (CRC) remains the second leading cause of cancer deaths in the United States (more than 57,000 projected deaths in 2009) despite the availability of sensitive screening tests such as colonoscopy. The inconvenience of the test and the risks involved contribute to the low adherence rate (40%) among U.S. adults. Our goal is to develop a noninvasive urine screening test for the early detection of adenoma and CRC that will enable more precise identification of individuals within the population who require colonoscopies. Such a test would enhance screening for CRC, reduce the cost to society of performing expensive, invasive diagnostic examinations that yield a majority of negative results, and ultimately save lives through early detection.
We successfully detected CRC-associated K-ras mutations in the urine of patients with CRC that are genetically heterogeneous. A single marker is unlikely to have sufficient sensitivity and specificity to be used as a stand-alone screening test. A panel of urine biomarkers that includes both genetic and epigenetic DNA alterations should provide a test with high sensitivity and specificity for CRC. In the past year, we have successfully developed a sensitive assay for detecting one of the most promising CRC DNA markers, aberrant hypermethylation of the vimentin gene, in the urine of patients with CRC. We performed a blinded study in which we used our assay to detect hypermethylated vimentin in 20 CRC tissue and 20 CRC urine samples identified only by barcodes. We did not know which tissue matched to which urine sample. As a control for healthy subjects, we also examined 20 urine DNA samples from subjects with no known neoplasia.
Using our assay, we detected methylated vimentin gene in 80% of CRC tissue samples and in 75% of urine samples with a concordance of 70% between marker-positive tissues and their matched urine samples. Ten percent of urine samples from control subjects contained a low level of methylated vimentin.
The results of this project indicate that, in addition to genetic mutation markers, epigenetic methylated DNA markers could also be used for a urine test. Work is in progress to develop a technology platform for screening a panel of CRC markers to develop a CRC screening test that would be acceptable to the high-risk population, thereby improving compliance. The availability of a noninvasive urine test would enhance the willingness of patients to undergo CRC screening, and CRC could be detected at an early, curable stage.
A manuscript describing the work is being prepared for publication.