Prostate Cancer
Bipolar Androgen Therapy: Breaking Out of the Chrysalis of Chronic Androgen Deprivation Therapy in Men with Late-Stage Castrate-Resistant Prostate Cancer



Posted June 23, 2020
Samuel Denmeade, Ph.D., Johns Hopkins University

Treatments to block or lower testosterone have been the standard therapy for prostate cancer since the seminal work of Charles Huggins on suppression of androgens in the 1940s. Men with prostate cancer are typically treated with androgen ablation therapy, however those treatments often stop working and result in the development of castration-resistant prostate cancer (CRPC). One way that this resistance may occur in these cells is adapting to a low testosterone environment while maintaining high levels of the androgen receptor. Paradoxically, studies have shown that CRPC cells can be growth-inhibited by treatment with extremely high levels of androgens. This novel and intriguing concept of using high dose testosterone as a therapy for prostate cancer seemed counterintuitive and was initially met with much skepticism. Dr. Samuel Denmeade and colleagues at Johns Hopkins University wanted to see if this different approach to therapy would work, and started by performing a small pilot clinical trial in which they learned that men with metastatic CRPC could tolerate FDA-approved doses of testosterone that produced high blood levels of testosterone without worsening side effects or causing disease progression. With this, the concept of bipolar androgen therapy (BAT) was established, which consists of a treatment strategy where CRPC cells rapidly cycle between supra physiological androgen levels and androgen ablation therapy.
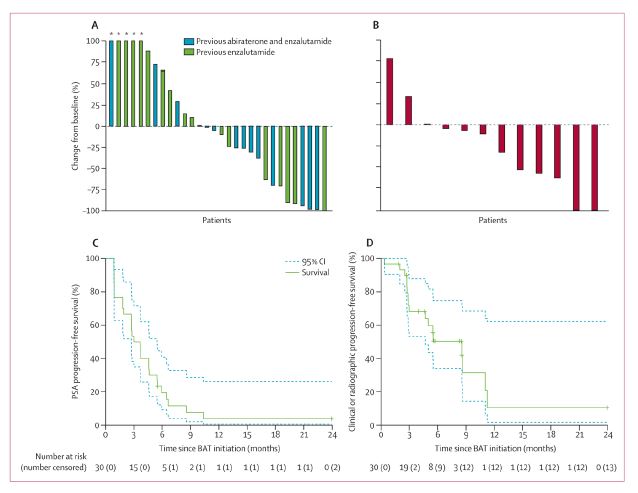
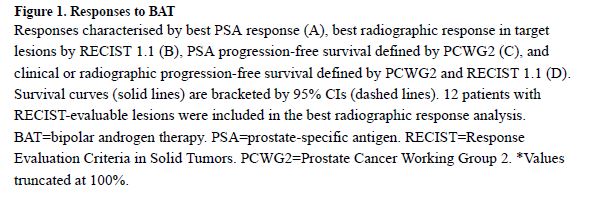
With support from a PCRP FY13 Transformative Impact Award, Dr. Denmeade and his team performed a clinical study to expand on their previous clinical results and demonstrate that high dose testosterone can be safely administered and produce a therapeutic effect in men with CRPC, increase their quality of life, and potentially re-sensitize them to androgen therapy. With this funding, they completed a randomized Phase II study comparing BAT with the androgen inhibitor enzalutamide in asymptomatic men with CRPC (NCT02286921). For this TRANSFORMER (Testosterone Revival Abolishes Negative Symptoms, Fosters Objective Response and Modulates Enzalutamide Resistance) trial, they recruited 200 men from 17 research sites around the country. Surprisingly, even though these two therapies are the exact opposite of each other, they observed remarkably similar effects in these men and demonstrated the same time to disease progression (5.7 months), indicating that BAT did not enhance disease progression. Interestingly, they found that while 25% of patients who received enzalutamide before BAT had an effective response to the treatment, the response rate for patients who received enzalutamide after BAT was 75%, and the duration of their response was three times longer meaning that it took longer for their PC to stop responding to treatment. Finally, they showed BAT can enhance quality of life and restore sexual function in some men.
These results suggest that in addition to a primary response from BAT treatment, high dose testosterone has the potential to increase the duration of response to androgen ablative therapies like enzalutamide and may enhance quality of life after treatment. Based on these findings, the JHU team recently received a FY19 PCRP Clinical Trial Award to evaluate the effectiveness of repeat cycling between BAT and enzalutamide to determine if this approach could extend the effectiveness of the therapy regimen while minimizing the side effects. The clinical trial is anticipated to begin in late 2020. The work of Dr. Denmeade and his team epitomizes the goal of the PCRP to support innovative research ideas that have the potential to make a significant impact on the lives of men living with prostate cancer – in this case not only giving patients a prolonged or potentially an indefinite response to therapy, but also improving their quality of life. The true impact of this work on patient care will continue to emerge as more studies are performed. However, the results from the TRANSFORMER study suggest we may need to modify the current hormone therapy paradigm to incorporate periods of high dose testosterone alternating with periods of androgen deprivation as a way to prolong the duration and magnitude of hormone response.
Publications:
John T. Isaacs, W. Nathaniel Brennen, and Samuel R. Denmeade. Rationale for bipolar androgen therapy (BAT) for metastatic prostate cancer. Cell Cycle, 2017, VOL. 16, NO. 18, 1639–1640.
Benjamin A Teply, MD, Hao Wang, PhD, Brandon Luber, MS, Rana Sullivan, RN, Irina Rifkind, RN, Ashley Bruns, RN, Avery Spitz, RN, Morgan DeCarli, BS, Victoria Sinibaldi, CRNP, Caroline F Pratz, CRNP, Changxue Lu, PhD, John L Silberstein, MHS, Jun Luo, PhD, Michael T Schweizer, MD, Prof Charles G Drake, MD, Prof Michael A Carducci, MD, Channing J Paller, MD, Emmanuel S Antonarakis, MD, Prof Mario A Eisenberger, MD, and Prof Samuel R Denmeade, MD. Bipolar androgen therapy in men with metastatic castration-resistant prostate cancer after progression on enzalutamide: an open-label, phase 2, multicohort study. Lancet Oncol. 2018 January; 19(1): 76–86.
Link:
Last updated Thursday, November 13, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
