Prostate Cancer
Autonomic Nerves Drive Prostate Cancer Growth, Invasion, and Metastasis



Posted September 14, 2018
Paul Frenette, M.D., Albert Einstein School of Medicine

Albert Einstein School of Medicine
Localized prostate cancer (PCa) is usually slow growing, but if the cancer begins to invade and metastasize to other parts of the body, most often to the bone, then prostate cancer quickly becomes lethal. If the process of invasion and metastasis is better understood, it is possible prostate cancer can be controlled and become a chronic, non-threatening disease. Dr. Paul S. Frenette and his colleagues then at Mount Sinai School of Medicine discovered an unexpected role for the nervous system in the invasion and metastasis of prostate cancer. Funded by a FY06 Idea Development Award, Dr. Frenette was able to further investigate this novel discovery, which has led to a better understanding of how the autonomic nervous system, which is responsible for regulating body functions such as heart rate, respiratory rate, urination, and sexual arousal, can also regulate PCa development and metastasis.
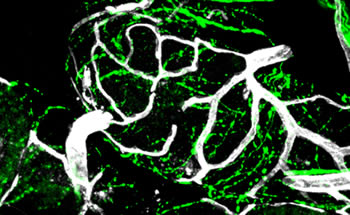
The autonomous nervous system consists of adrenergic nerves of the sympathetic nervous system, and cholinergic nerves of the parasympathetic nervous system. Interestingly, Dr. Frenette's group uncovered distinct functions for each set of autonomous nerves in controlling PCa growth; while adrenergic signals control the early phases of cancer development, cholinergic signals play important roles in tumor cell invasion and metastasis. Through a retrospective blinded analysis of PCa specimens from 43 patients, they revealed that increased densities of sympathetic and parasympathetic nerve fibers in tumor and surrounding normal tissue were associated with poor clinical outcomes. In further studies, they found that denervation (loss in nerve supply) of adrenergic nerves prevented the development of blood vessels and subsequently PCa growth. They also discovered that expression of the beta2 adrenergic receptor (Adrb2) acted as a nerve-dependent angiogenic 'switch' in endothelial cells. If this switch is turned off by deleting Adrb2, a cascade of events including changes in Coa6 expression and metabolism leads to inhibited angiogenesis and tumor growth. These results suggest a novel interplay between neural signals, tumor metabolism, and angiogenesis.
Dr. Frenette's work suggests that blocking Adrb2 through a non-specific beta blocker in PCa patients could inhibit tumor growth. Now located at Albert Einstein School of Medicine, Dr. Frenette and his clinical collaborators at Montefiore have begun a pilot study in PCa patients who are receiving a non-selective beta blocker after their diagnostic biopsies and prior to their prostatectomy. They will evaluate the impact of the beta blocker on tumor proliferation, cell death markers, and innervation. This Montefiore-Einstein pilot study titled "Beta adrenergic receptor blockade as a novel therapy for patients with adenocarcinoma of the prostate," is led by Benjamin Gartrell, M.D., and can be found on the website ClinicalTrials.gov (NCT02944201).
Publication:
Magnon C, Hall S, Lin J, et al. 2013. Autonomic Nerve Development Contributes to Prostate Cancer Progression. Science.
Zahalka A, Arnal-Estapa A, Maryanovich M et al. 2017. Adrenergic nerves activate an angio-metabolic switch in prostate cancer. Science.
Link:
Neural Control of Prostate Cancer Metastasis
Last updated Monday, March 10, 2025














