Prostate Cancer
Prostate Cancer PET Biopsies: Painless Precision Medicine



Posted September 13, 2017
Michael Evans, Ph.D., University of California, San Francisco

University of California, San Francisco
The FDA approval of two potent androgen receptor (AR) inhibitors, abiraterone acetate and enzalutamide, for the treatment of advanced prostate cancer (PCa) was a milestone for the disease. Unfortunately, virtually all targeted therapies have transient effects in humans and treatment resistant tumors emerge typically within months after the start of therapy. Because targeted therapies are often applied to patients with very advanced metastatic cancers, determining if the drug target is completely inhibited in cancer cells cannot be easily done with an invasive biopsy. Biopsy may not always recover tumor tissue since metastases are small, and there can be reluctance from patients to submit to a high risk and painful invasive procedure. Therefore, new non-invasive methods must be developed to better understand PCa tumor biology.
With support from a FY14 Idea Development Award, Dr. Michael Evans at the University of California, San Francisco (UCSF) is developing imaging technologies for positron emission tomography (PET) that can detect molecular drivers within tumor cells, with a special emphasis on those drivers that are also "druggable". Dr. Evans and his colleagues have coined this technology "PET biopsies", which has several advantages over a standard needle biopsy. First, they are able to measure the downstream action of druggable cancer drivers to prospectively identify patients whose tumors might respond to a certain targeted therapy. Second, "PET biopsies" are safe and reliable for repeated patient use, enabling doctors to measure the efficacy of a targeted therapy over time. Lastly, the specificity of "PET biopsies" for detecting specific tumor indicators may help better distinguish aggressive PCa from indolent forms that may not require treatment.
Dr. Evans' research group has already translated iron-based "PET biopsies" into patients with PCa. They were able to detect biological differences, or heterogeneity, among metastases within the same patient, and they have integrated this PET scan into a MYC inhibitor clinical trial. The post-therapy PET scans of patients have shown decreased uptake of the iron-based PET probe, suggesting effective drug activity; they are now working to understand the clinical significance of these post-treatment changes.
Dr. Evans and his colleagues are pioneering the development of PET scans to measure individual cancer drivers for tumor detection and treatment monitoring, and note that many research and treatment centers have the infrastructure to achieve the type of work that they are doing. They plan to continue developing new "PET biopsies" for other major drivers of PCa that may reach the clinic within the next five years, and they hope that others will join them in developing the "PET biopsy" concept, as it holds high promise for improving precision medicine in PCa.
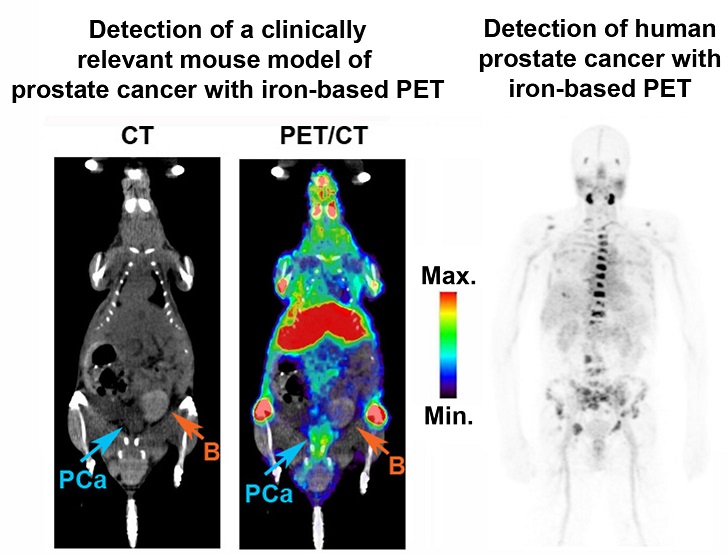
Performing a "PET biopsy" of PCa with iron-based PET. Left: A representative image of a genetically engineered mouse with hyperactive mTORC1 in the prostate cancer cells (PCa) taken 48 hours after initiating the iron based PET study shows a high signal in the PCa tumor. B = bladder. Right: A representative image of a patient with castration resistant PCa with several bone metastases that are detected using iron-based PET. Several metastases observed on standard of care imaging were not avid on the PET scan, which indicates that this patient's tumors are likely biologically heterogeneous.
Link:
Last updated Monday, March 10, 2025














