


Posted April 21, 2015
Gyorgy Petrovics, Ph.D., Uniformed Services University of the Health Sciences
 Although it is well known that there is a striking disparity in prostate cancer incidence and mortality for African American (AA) men as compared with Caucasian Americans (CA), the biological basis for it has not yet been established. Evidence suggests that diet, hormones, and genes may all play a role in this ethnic disparity. The most common genetic alteration found in prostate cancer is a chromosomal translocation that results in an abnormal fusion of two genes, TMPRSS2 and the proto-oncogene ERG, resulting in the TMPRSS2-ERG fusion protein, which is critical for the progression of prostate cancer. Dr. Gyorgy Petrovics, working with a group of researchers at the Center for Prostate Disease Research, has been investigating the ERG expression status in a large number of prostate tumors from the Walter Reed National Military Medical Center's Biospecimen Bank, which contains comprehensive information on 28,000 beneficiaries, with equal access to the military health system, who have had a prostate biopsy, about 25% of whom are AA men.
Although it is well known that there is a striking disparity in prostate cancer incidence and mortality for African American (AA) men as compared with Caucasian Americans (CA), the biological basis for it has not yet been established. Evidence suggests that diet, hormones, and genes may all play a role in this ethnic disparity. The most common genetic alteration found in prostate cancer is a chromosomal translocation that results in an abnormal fusion of two genes, TMPRSS2 and the proto-oncogene ERG, resulting in the TMPRSS2-ERG fusion protein, which is critical for the progression of prostate cancer. Dr. Gyorgy Petrovics, working with a group of researchers at the Center for Prostate Disease Research, has been investigating the ERG expression status in a large number of prostate tumors from the Walter Reed National Military Medical Center's Biospecimen Bank, which contains comprehensive information on 28,000 beneficiaries, with equal access to the military health system, who have had a prostate biopsy, about 25% of whom are AA men.
In a recently published study, Dr. Petrovics with support from a FY12 PCRP Health Disparity Research Award made the startling finding that ERG expression - examined in a cohort of 126 patients (63 CA and 63 AA) - was three times more likely to be present in the high-grade tumors of Caucasian patients (49%) than in those of AA men (16%) (P<0.0001). Thus, although ERG may be the most common oncogenic alteration in aggressive tumors from CA patients, that does not appear to be the case in aggressive tumors from AA patients. The data suggest that ERG is not the primary driver of aggressive disease in AA men, so the question now is, if ERG is not to blame, what is?
To answer that question, Dr. Petrovics is now trying to identify common genetic alterations, including both somatic mutations (present in tumor cells) and inherited genetic variations (present in all cells), in AA patients with aggressive prostate cancer. That knowledge will help guide the development of rationally designed, personalized treatment strategies into the clinic with the goal of eventually eliminating prostate cancer-related disparities.
Left side:
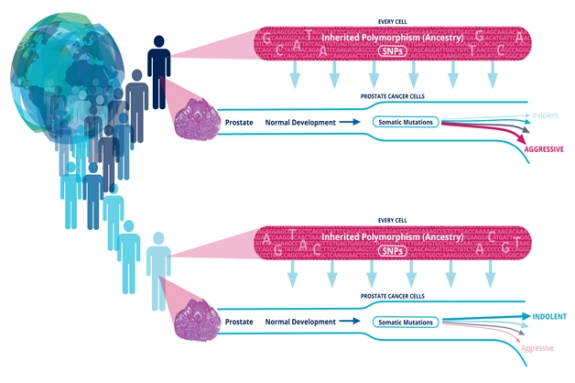
Different shades represent people with different ancestry (ethnicity) with the globe as a background
Right side:
Upper panels (red blocks): People with different ancestry have different inherited single nucleotide polymorphisms (SNPs) in every cell of their body (two examples shown).
Lower panels (prostate cancer development flows): Some of the SNPs may affect prostate cancer development, therefore contributing to the disparate burden of the disease in people with different ancestry, e.g. African (upper example) versus Caucasian (lower example).
Collecting this important SNP information is simple (from small blood sample) and can be done very early (present already at birth). Complementing clinical, pathological and other molecular (somatic mutations) characteristics with inherited SNP data will provide more complete information for the clinician and the patient in managing the disease and in decreasing disparity by personalizing prevention and treatment strategies.
Publication:
Farrell J, Young D, Chen Y, Cullen J, Rosner IL, Kagan J, Srivastava S, McLeod DG, Sesterhenn IA, Srivastava S, Petrovics G. 2014. Predominance of ERG-negative high-grade prostate cancers in African American men. Molecular and Clinical Oncology 2(6):982-986.
Link:














