


Posted May 18, 2015
Renée de Leeuw, Ph.D., Thomas Jefferson University
 In 2010, the FDA approved next-generation taxane-based chemotherapy, cabazitaxel (Jevtana®), for patients with metastatic castration-resistant prostate cancer (CRPC) whose cancer no longer responds to androgen deprivation therapy (ADT) or docetaxel, the previous generation taxane-based chemotherapy. Under the mentorship of Dr. Karen Knudsen, and with funding from a Fiscal Year 2012 PCRP Postdoctoral Training Award, Dr. Renée de Leeuw explored how cabazitaxel works, and why it works where docetaxel fails.
In 2010, the FDA approved next-generation taxane-based chemotherapy, cabazitaxel (Jevtana®), for patients with metastatic castration-resistant prostate cancer (CRPC) whose cancer no longer responds to androgen deprivation therapy (ADT) or docetaxel, the previous generation taxane-based chemotherapy. Under the mentorship of Dr. Karen Knudsen, and with funding from a Fiscal Year 2012 PCRP Postdoctoral Training Award, Dr. Renée de Leeuw explored how cabazitaxel works, and why it works where docetaxel fails.
In studies of prostate cancer cells that are killed by (sensitive to) ADT, Dr. de Leeuw showed that cabazitaxel and docetaxel are relatively equivalent in their ability to curb cell proliferation and kill prostate cancer cells. Surprisingly, this was not the case for prostate cancer cells that are resistant to ADT; instead she found that cabazitaxel was much more effective than docetaxel at killing this type prostate cancer.
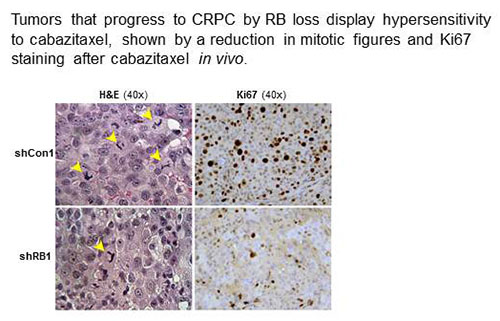
It turns out that tumors from patients who develop resistance to ADT frequently (about 60% of the time) lose a protein, first identified in childhood eye tumors, called the retinoblastoma tumor suppressor protein (RB). To study the possible role of RB loss in response to cabazitaxel treatment, Dr. de Leeuw took prostate cancer cells that are sensitive to ADT and removed the RB. Mice were injected with these RB-negative cells or with the original RB-positive cells, tumors were allowed to grow, and then the mice were treated with ADT (in this case, castration). A week later, the mice began treatment with cabazitaxel. Remarkably, Dr. de Leeuw found that after 2-3 weeks of cabazitaxel treatment, RB-negative tumors stopped growing, whereas RB-positive tumors kept growing, thus demonstrating that RB-deficient tumors are sensitive and RB-positive tumors are resistant to cabazitaxel treatment.
These results provided the rationale behind several new multicenter phase II clinical trials using RB as a biomarker for identifying patients who are likely to respond to cabazitaxel treatment and those not likely to respond. This could be a significant step toward precision medicine for prostate cancer patients. Dr. de Leeuw concludes that "this training award has given me the unique opportunity to see my project advance from bench to bedside, interact with cancer experts with different backgrounds, and provided me with better insight in what it takes to make laboratory ideas come to fruition, and ultimately improve treatment for cancer patients."
Research Links:
Links:














