


Posted March 11, 2014
Min Xu, Ph.D., Fairfield University
 Diagnosis and prognosis of prostate cancer from biopsy or prostatectomy specimens currently rely on histopathological evaluation to determine grade, stage, and surgical margin status. The Gleason score (GS) is the single most important prognostic factor in prostate cancer. It is one determinant of a patient's specific risk of dying from prostate cancer and strongly influences decisions regarding options for therapy. The majority of patients are now diagnosed with tumors of GS 6 and 7 and these tumors can take two distinct disease courses: indolent or highly aggressive, the latter of which leads to death if not treated. Although the GS is currently the most useful indicator for prognosis, it remains largely subjective. Furthermore, prostatic tissue must be removed in order to determine a GS, making the process invasive and therefore not ideal.
Diagnosis and prognosis of prostate cancer from biopsy or prostatectomy specimens currently rely on histopathological evaluation to determine grade, stage, and surgical margin status. The Gleason score (GS) is the single most important prognostic factor in prostate cancer. It is one determinant of a patient's specific risk of dying from prostate cancer and strongly influences decisions regarding options for therapy. The majority of patients are now diagnosed with tumors of GS 6 and 7 and these tumors can take two distinct disease courses: indolent or highly aggressive, the latter of which leads to death if not treated. Although the GS is currently the most useful indicator for prognosis, it remains largely subjective. Furthermore, prostatic tissue must be removed in order to determine a GS, making the process invasive and therefore not ideal.
To overcome this problem, Dr. Min Xu, with funding from an FY09 PCRP New Investigator Award, is utilizing light backscattering, the diffuse reflection of light back in the direction of the source, to identify correlations between optical tumor characteristics, prostate cancer grade, and patient outcome. To accomplish this, the PI developed an enhanced backscattering tomography technique that generates a three-dimensional map of tissue cellular architecture and nuclear morphology based on light scattering. This system is sensitive enough to quantify subtle changes in tissue architecture and nuclear structure that accompany tumor initiation and progression. Using tissue microarrays (TMAs) constructed by Dr. Jonathan Melamed's group at New York University, which was developed as part of the PCRP-funded Prostate Cancer Biorepository Network, Dr. Xu discovered that the optical characteristics of the nuclear region could be used to distinguish aggressive from indolent prostate cancer.
In hopes of bringing this research closer to helping current cancer patients, Dr. Xu is measuring more cohorts of prostate cancer TMAs and will further validate the correlations between the optical parameters with the grade of cancer and patient outcome. The PI also plans to develop an optical risk score for prostate cancer diagnosis and prognosis at the end of the funding period. In sum, Dr. Xu's research is laying the groundwork for constructing a noninvasive tool to help clinicians determine the most appropriate treatment strategy for protecting both life and quality of life for individual patients.
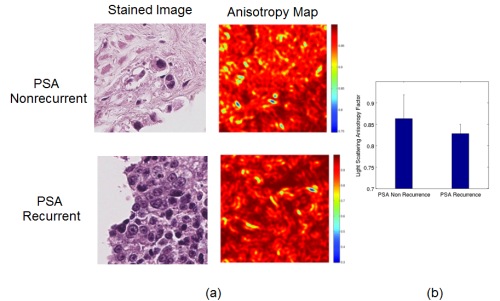
The light scattering anisotropy factor g, which describes the distribution of the direction of light being scattered by the structure, correlates strongly with prostate cancer aggressiveness. (a) shows the typical stained image and the anisotropy map for one non-aggressive prostate cancer (PSA non-recurrence within 5 yrs, top row) and one aggressive one (PSA recurrence within 5yrs, bottom row). The Gleason Score for both cases is 8. The average g over the nuclear region is 0.914 for the former and 0.779 for the latter. The window size is 100µm´100µm. (b) shows the average nuclear g is significantly smaller (p < 10-5), in general, for more aggressive prostate cancer than non-aggressive ones from our study on about 175 cases contained on the TMA slides.
Publications:
Links:
Last updated Thursday, December 5, 2024














