


Posted July 16, 2013
Barry Rosenstein, Ph.D., Mount Sinai School of Medicine
Harry Ostrer, M.D., Albert Einstein College of Medicine
 Great advances have been made in recent years to improve radiation therapy for prostate cancer. One such improvement involves being able to more specifically limit the radiation dose to the prostate cancer tissue, meaning that normal tissues can be better protected from the damaging effects of the radiation therapy. However, even with the improvements made, some amount of normal tissue still receives a substantial dose of radiation during the course of therapy. This exposure can result in toxicity that compromises urinary, rectal or sexual function. In addition, these toxicities can vary between patients who receive seemingly identical radiation treatment, leading to the hypothesis that genetic factors may influence radiation response. Therefore, Dr. Barry Rosenstein at the Mount Sinai School of Medicine and Dr. Harry Ostrer at the Albert Einstein College of Medicine have been working together to create an assay based upon personal data and genetic markers capable of predicting which men are at greatest risk for developing complications after prostate cancer radiotherapy.
Great advances have been made in recent years to improve radiation therapy for prostate cancer. One such improvement involves being able to more specifically limit the radiation dose to the prostate cancer tissue, meaning that normal tissues can be better protected from the damaging effects of the radiation therapy. However, even with the improvements made, some amount of normal tissue still receives a substantial dose of radiation during the course of therapy. This exposure can result in toxicity that compromises urinary, rectal or sexual function. In addition, these toxicities can vary between patients who receive seemingly identical radiation treatment, leading to the hypothesis that genetic factors may influence radiation response. Therefore, Dr. Barry Rosenstein at the Mount Sinai School of Medicine and Dr. Harry Ostrer at the Albert Einstein College of Medicine have been working together to create an assay based upon personal data and genetic markers capable of predicting which men are at greatest risk for developing complications after prostate cancer radiotherapy.
With support from a FY07 PCRP Synergistic Idea Development Award, they have been able to successfully identify over 100 different genetic markers, called single nucleotide polymorphisms (SNPs), that correlate with adverse effects upon urinary, rectal, and sexual function in patients treated with radiation therapy. By bringing together a team of investigators with a wide range of scientific and clinical expertise in areas such as radiation biology, radiation oncology, genomics, and urology, Drs. Rosenstein and Ostrer have created a research group capable of translating these types of findings from the lab to the clinic. And, as leaders in the field of "radiogenomics," they have also worked to create the international Radiogenomics Consortium (RGC), including 157 investigators at 82 institutions in 19 countries, for the purpose of sharing biospecimens and data, enabling the type of large scale studies essential for development of a predictive assay. With these types of translational resources, Drs. Rosenstein and Ostrer plan to complete the development of a robust, validated, sensitive, and specific clinical assay capable of predicting the risk for development of erectile dysfunction, urinary morbidity or rectal injury following radiation treatment for prostate cancer, which will have a major impact on improving the survivorship and well-being of the millions of men undergoing treatment for prostate cancer.
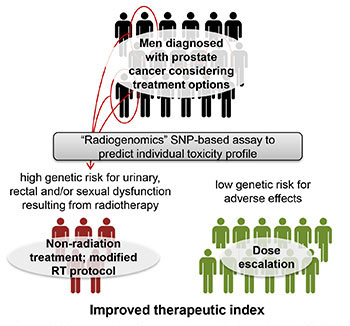
A predictive assay based on genetics could be used to identify the subset of patients at increased risk of developing adverse effects. These patients could be candidates for a non-radiation treatment, such as surgery, or active surveillance. Patients who do not have a genetic predisposition to adverse effects could receive a higher dose to increase likelihood of curing their cancer.














