


Posted October 16, 2013
Gregory J. Czarnota, Sunnybrook Health Sciences Centre
 Radiation therapy remains a vital tool in the treatment of cancer - over half of all patients diagnosed with cancer receive radiation therapy. But the high doses of radiation needed to kill cancer cells also damage normal cells and, despite efforts to localize treatment and minimize side effects, radiation therapy remains far from ideal.
Radiation therapy remains a vital tool in the treatment of cancer - over half of all patients diagnosed with cancer receive radiation therapy. But the high doses of radiation needed to kill cancer cells also damage normal cells and, despite efforts to localize treatment and minimize side effects, radiation therapy remains far from ideal.
A new technique is currently being developed by scientists at the University of Toronto that works synergistically to boost radiation's tumor-killing power. With the same efficacy at lower doses, the technique has the potential to provide patients effective treatment while minimizing harm to their body's healthy cells.
The imaginative approach employs tiny spheres called microbubbles and ultrasound to vibrate them. Today, ultrasound and microbubbles are already commonly used in contrast-enhanced ultrasound imaging of vasculature. The microbubbles are micron-sized spheres. The microbubble sphere is composed of stabilizing material, such as a protein or liquid, and contains gas, typically a perfluorocarbon. With a median diameter of about 3 µm they are comparable in size to red blood cells and thus small enough to pass systemic circulation after being injected peripherally. In imaging their job is to act as intravascular reflectors of ultrasound and increase the contrast for better resolution of the blood vessels they fill. The research team, led by Dr. Gregory J. Czarnota, discovered that vibrating microbubbles at certain ultrasound frequencies can induce apoptosis in blood vessel cells they are in contact with.
Radiation works primarily by damaging cancer cell DNA. Scientists have recently found, however, that radiation also induces apoptosis in the endothelial cells that line the inner surface of tumor blood vessels. Vibrating microbubbles add to this by acting as small battering rams, mechanically disrupting the endothelial cells of tumor vasculature and inducing apoptotic cell death. The vascular destruction that follows leads to decreased blood flow to the tumor and secondary tumor cell death. In a 2012 study published in PNAS, Czarnota's group showed that combining ultrasound-stimulated microbubble vascular disruption with radiation resulted in a 10-fold greater number of tumor cells killed than with radiation alone.
Dr. Czarnota talks about the work, funded by both the Breast Cancer Research Program and Prostate Cancer Research Program, which led to the development of this promising technique:
What is the most important thing(s) that breast and prostate cancer researchers should know about your BCRP-/PCRP-funded research?
Breast and prostate cancer researchers should know that the BCRP-/PCRP-funded research has led to some important discoveries about treatment enhancements in radiation oncology by using ultrasound-stimulated microbubbles. We have demonstrated that low mechanical-index ultrasound mediated excitation of microbubbles intravascularly can enhance tumor-killing by 40% when compared to just radiation doses alone in our preclinical testing of breast and prostate cancers. Furthermore, we have demonstrated that blood vessels play an important role in tumor-radiation response. These findings have the promise of reshaping how we treat cancer patients with breast and prostate cancer in radiation oncology.
What is the most important thing(s) that breast and prostate cancer survivors should know about your research?
The most important things that breast and prostate cancer survivors should know about our research are that our emerging treatment discoveries could help change the way we treat breast and prostate cancers in the near future. In many clinical situations where radiation is used for prostate and breast cancer, our preclinical testing has yielded biomedical science advancing discoveries that will translate to fewer side effects from radiation treatment and a reduction in the number of visits required to the hospital for treatment.
What led you to this research question?
As clinicians, it is important that we find new ways in order to better the lives of our patients. This research question emerged from recent paradigm shifts that have given us clues about the interactions of radiation and tumor blood vessels. These clues have driven our research in this direction.
How is your research accelerating progress toward ending breast and prostate cancer (including the potential short-term and long-term impact)?
Our research is accelerating progress toward ending breast and prostate cancer through our innovations in cancer therapies. Radiation is a major anti-cancer therapy and is currently used to treat a majority of patients with tumors and our research is finding ways towards better and more effective treatments that can potentially eradicate tumors or increase the potency of radiation treatments.
How have your BCRP and PCRP funding helped advance your microbubble research?
The BCRP and PCRP funding has helped to advance our research tremendously by allowing for resources to be focused on discovery and optimization. Through these important funding opportunities, we were able to ensure the sustainability of work that our trainees and researchers rigorously took upon to find translatable outcomes into clinical applications. The BCRP and PCRP funding has also given us vital opportunities to further explore the underlying biological foundations of tumor vessel signals and how these signals are integral to escalating radiation damage to prostate and breast tumors. The funding was crucial to start and sustain what was high-risk, groundbreaking new research.
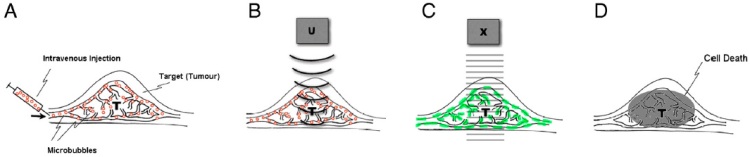
Ultrasound-stimulated microbubbles injected into tumors cause tumor-blood vessel disruption. When combined with radiation, tumors demonstrate a 40% increase in tumor cell death.
Reference: Proc Natl Acad Sci U S A. 2012 Jul 24;109(30):E2033-41














