Multiple Sclerosis
Mitochondrial Dysfunction and Disease Progression in MS



Posted August 2, 2019
Patrizia Casaccia, M.D., Ph.D., Icahn School of Medicine at Mount Sinai and Advanced Science Research Center (ASRC) at The Graduate Center of The City University of New York
Ilana Katz Sand, M.D., Icahn School of Medicine at Mount Sinai
Catarina Quinzii, M.D., Columbia University, Medical Center



Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease of the central nervous system, characterized by lesions and an underlying neurodegenerative process. Clinically, MS is categorized into three phenotypes according to the disease course: relapsing remitting (RRMS), secondary progressive (SPMS), and primary progressive (PPMS). Approximately 85% of people with MS are initially diagnosed with RRMS, which is characterized by acute episodes of focal neurologic dysfunction followed by periods of clinical remission. However, approximately 50% of RRMS patients later develop progressive neurological decline indicating transition to the SPMS phenotype. In addition, the remaining 15% of MS patients are classified as PPMS at disease onset, presenting with progressive neurological deterioration from the start. Progressive disease is responsible for the majority of MS-related disability over time and therapeutic options are very limited, highlighting the need to improve our knowledge of pathophysiology to drive targeted treatment development. While it has been proposed that mitochondrial dysfunction underlies this neuronal damage, our understanding of the precise molecular and cellular mechanisms by which this occurs remains incomplete.
With support from a Fiscal Year 2014 Investigator-Initiated Partnership Award, Dr. Casaccia - who currently directs the Neuroscience Initiative at the ASRC - along with her colleagues Dr. Katz Sand and Dr. Matilde Inglese at the Icahn School of Medicine, Dr. Quinzii at Columbia University, Medical Center, and Dr. Valentina Fossati at the New York Stem Cell Foundation, have been studying how extrinsic and cell intrinsic factors modulate neuronal bioenergetics, potentially contributing to MS progression. In a recent Brain publication, the authors described how they conducted a morphological and functional screening of mitochondria in neurons exposed to the cerebrospinal fluid (CSF) of MS patients with a relapsing remitting or a progressive disease course. They found that exposure to the CSF of progressive MS patients, but not relapsing-remitting MS patients or healthy individuals, induced elongated tubular structures in neuronal mitochondria that were reminiscent of the mitochondrial morphology exposed to conditions of decreased nutrient availability.
Furthermore, they observed increased phosphorylation of the protein DRP1 and mitochondrial fusion in neurons treated with the CSF of PPMS patients but not RRMS patients. Mitochondrial fusion has been reported as a form of adaptation to environmental challenges by providing a functional advantage to cells by rejuvenation and increased energy production. Unfortunately, instead of being associated with increased energy production, the mitochondrial fusion induced by the CSF from progressive patients was also associated with impaired activity of the respiratory chain complexes I, III, and IV, decreased oxygen consumption rate and energy production by the mitochondria, which eventually led to axonal damage. In addition, the lipid with the most significant differential abundance in the CSF of progressive compared to relapsing-remitting patients was ceramide C24. Treatment of neurons with C24 had two effects: it directly impaired mitochondrial function and it also induced a transcriptional response which led to the increased production of glucose transporters. The data suggested that neurons may compensate to inefficient energy production by attempting to incorporate more glucose, although they are unable to use it effectively to generate the much needed energy for proper function. This condition, called by the authors as “virtual hypoglycosis,” describes a marked energetic deficit and neurotoxicity, even in the presence of physiological levels of glucose. All those changes were reminiscent of the neuronal response to exposure to CSF samples from progressive patients. Taken together, these data suggest that exposure of neurons to factors present in the CSF of patients with a progressive MS leads to a maladaptive mitochondrial response, pointing to the “virtual hypoglycosis” condition as the underlying basis for neurodegeneration in progressive MS.
Currently the team is deriving neurons from induced pluripotent stem cells from MS patients and plans to characterize their mitochondrial function. If successful, the researchers will advance the current knowledge of the progressive forms of MS laying the groundwork for the identification of potential therapeutic targets for progression and the identification of potential biomarkers predictive of disease course.
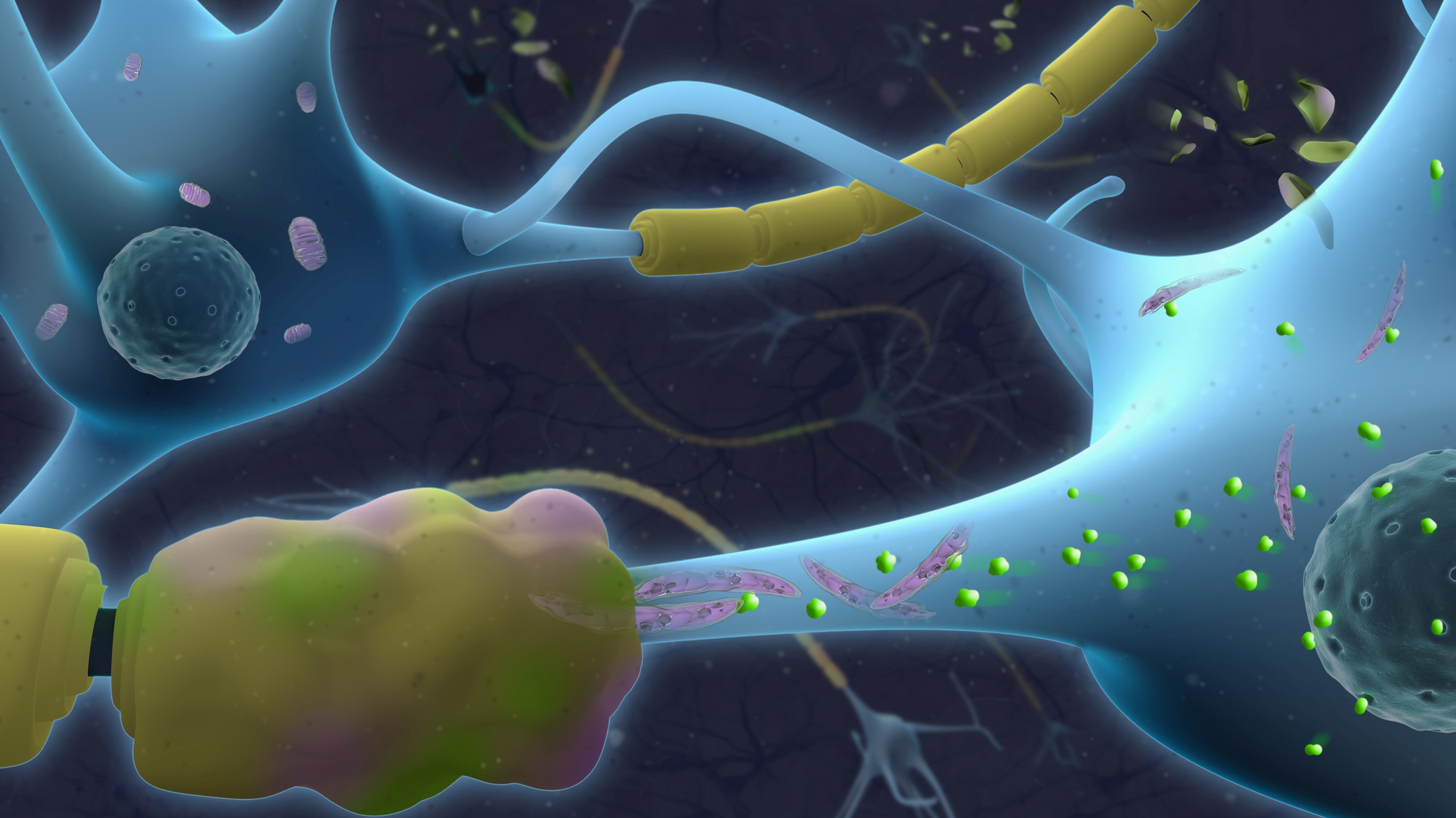
The top portion of this graphic features neurons (blue) with axons wrapped by normal myelin (yellow). The lower portion of this graphic illustrates neurons with pathological axons wrapped by damaged myelin (yellow and pink). The elongated mitochondria (purple) in the lower portion are dysfunctional and characterized by accumulation of toxic ceramides (green).
Reference:
Wentling M, Lopez-Gomez C, Park HJ, et al. 2019. A metabolic perspective on CSF-mediated neurodegeneration in multiple sclerosis. Brain. doi: 10.1093/brain/awz201. [Epub ahead of print July 15, 2019]
Link:
Public and Technical Abstracts: Mitochondrial Dysfunction and Disease Progression
Last updated Thursday, December 5, 2024














