Melanoma



Posted May 10, 2022
May is Melanoma and Skin Cancer Awareness Month. In support of the awareness efforts, the Melanoma Research Program (MRP) will run a series of features this month highlighting some exciting new initiatives from the program and the people without whom the MRP could not achieve its Vision. This installment describes the MRP's latest efforts to address unmet needs in the rare melanoma community.
When most people hear "melanoma” they likely think of superficial spreading melanoma, a type of cutaneous melanoma that accounts for 70% of all melanomas.1 Some of the defining characteristics of this form of melanoma include exposure to ultraviolet (UV) radiation as a primary risk factor, tumor cells that have DNA with large numbers of mutation (i.e., a high tumor mutation burden [TMB]), and that many patients will respond well to immunotherapy treatments. However, the remaining 30% of melanoma diagnoses are comprised of several subtypes of melanoma collectively referred to as "rare melanomas.”
Rare melanomas can have distinct characteristics compared to superficial spreading melanoma. For certain rare melanomas, like uveal melanoma (UM), acral letiginous melanoma (ALM), and mucosal melanoma (MM), exposure to UV light is not thought to be a primary risk factor. However, little is known about what the risk factors are for these types of melanoma. UM is the most common form of eye cancer, with approximately 2,000-2,500 new cases diagnosed in the United States (U.S) each year, with more than 70% of UM lesions arising from existing uveal nevi (i.e., moles in the eye). But most uveal nevi will not transform into UM, and the mechanisms that drive the formation of the other 30% of UM cases are not understood. ALM develops on the palms of hands, soles of feet, or under the nail beds. Although it is a rare diagnosis for Caucasians, ALM is the predominant cause of melanoma in persons with darker skin, a factor of note, considering that approximate 40% of the U.S. active-duty military members are racial and ethnic minority groups.2 MM is particularly challenging to diagnose, as it arises in mucosal tissues such as those lining the nasal passages, vagina, or gastrointestinal track; subsequently, it is frequently diagnosed at later, more difficult to treat, stages of disease. A shared characteristic across these rare melanomas that sets them apart from the more commonly diagnosed cutaneous melanomas is that these tumor cells have a much lower TMB, and therefore are less likely to respond well to immunotherapy treatments. However, alternative, more effective treatment strategies are unknown. This is just a brief overview of a few examples of rare melanomas. Other types, such as amelanotic melanoma (melanoma that lacks pigmentation), pediatric melanoma, etc., also present with their own prevention, diagnosis, and treatment challenges. Overall, rare melanomas are less well-studied than superficial spreading melanomas, leading to a dearth in knowledge across the entire cancer research spectrum (Figure 1).
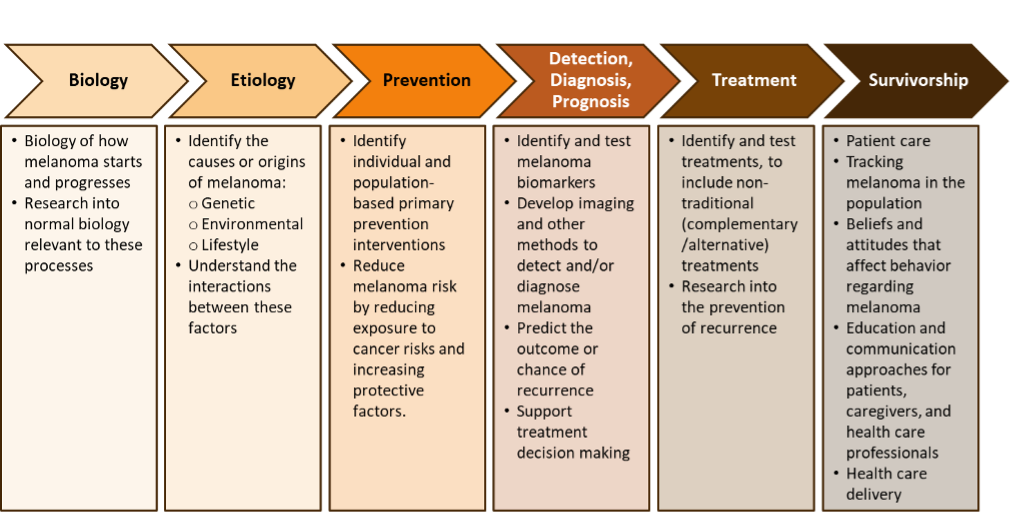 Figure 1: The cancer research spectrum represents the Common Scientific Outline (CSO).3 The CSO is a coding system developed by the International Cancer Research Partnership and is used by cancer-funding organizations across the world to allow for easy comparisons of cancer research portfolios across agencies.
Figure 1: The cancer research spectrum represents the Common Scientific Outline (CSO).3 The CSO is a coding system developed by the International Cancer Research Partnership and is used by cancer-funding organizations across the world to allow for easy comparisons of cancer research portfolios across agencies.
Every application to the MRP, in addition to answering the MRP Challenge Statement, must address at least one Focus Area that promotes the role of prevention throughout the melanoma disease process. To encourage applications that respond to the critical unmet needs of the rare melanoma community, the MRP has added the following Focus Area in all fiscal year 2022 (FY22) funding opportunities:
Additionally, in FY22 the MRP is introducing a new funding opportunity for the program, the Focused Program Award - Rare Melanomas (FPA-RM). The intent of this exciting opportunity is to bring together a team of 2-3 investigators to optimize their research efforts and accelerate solutions for an overarching challenge or question critical to the needs of the rare melanoma consumer community (Figure 2). The projects may range from exploratory/hypothesis-developing through small-scale clinical trials that together will address the overarching challenge/question.
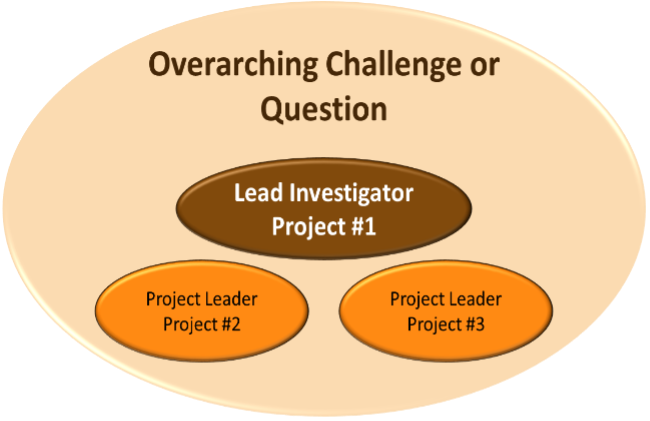 Figure 2: Infographic representing one example of a FPA-RM project team.
Figure 2: Infographic representing one example of a FPA-RM project team.
The MRP also recognizes that melanoma patients, survivors, and caregivers can provide important perspectives to the design of both laboratory and clinical research (Figure 3).4,5 Applicants to the FPA-RM are encouraged to employ a rare melanoma community collaborative approach to optimize the impact of the research for this community. This collaborative approach can be approached in several ways. The following are a few options for incorporating the rare melanoma patient voice into the project, but the research teams may explore other options as appropriate for the overarching challenge/question being explored.
- The research team includes at least one advisor with lived rare melanoma experience who will provide advice and consultation throughout the planning and implementation of the research project. Lived experience advisors may include rare melanoma patients/survivors, their family members, or caregivers.
- The research team establishes partnerships with at least one community-based organization that provides advice and consultation throughout the planning and implementation of the research project. Community-based organizations may include advocacy groups, policy makers, or other formal organizational stakeholders.
- The research team assembles a community advisory board composed of multiple community stakeholders. This advisory board can take many forms, from a board of advisors with lived rare melanoma experience to a coalition of community-based organizations, or any combination thereof. As with individual lived experience advisors and organizational partners, the community advisory board provides advice and consultation throughout the planning and implementation of the research project.
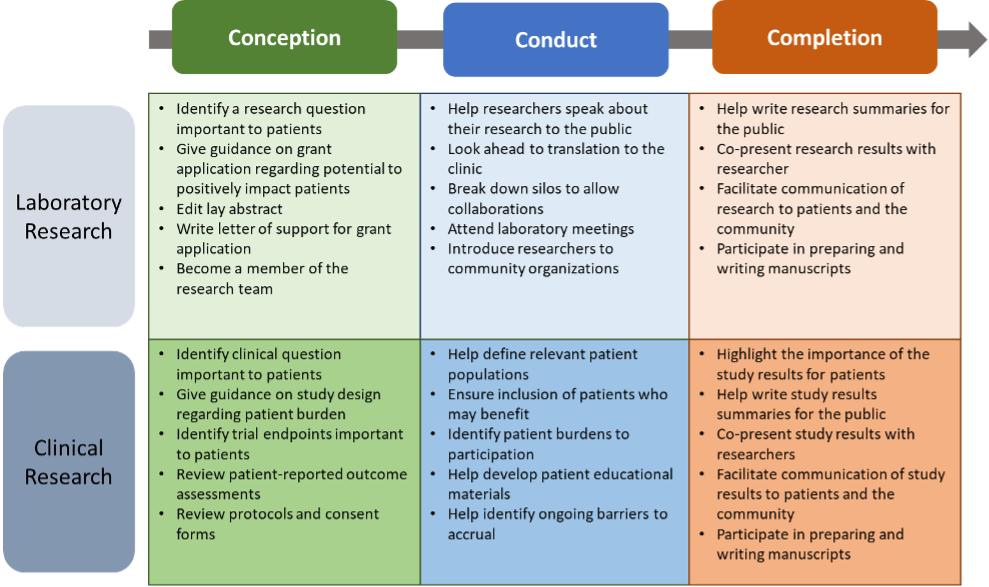 Figure 3: Originally published in Spears,4 the table above elaborates on how the voice of patient advocates can be incorporated through the duration of a laboratory or clinical project.
Figure 3: Originally published in Spears,4 the table above elaborates on how the voice of patient advocates can be incorporated through the duration of a laboratory or clinical project.
The MRP looks forward to receiving proposals from a diverse group of applicants that rise to the challenge of promoting the role of prevention throughout the melanoma disease process and address the unmet needs of the rare melanoma communities.
Note for readers: Abstracts for all previously funded MRP awards can be viewed at, https://cdmrp.health.mil/search.
References:
1SEER Training Modules. National Cancer Institute. https://training.seer.cancer.gov/melanoma/.
2Pew Research Center. 6 facts about the U.S. military and its changing demographics. https://www.pewresearch.org/fact-tank/2017/04/13/6-facts-about-the-u-s-military-and-its-changing-demographics/.
3International Cancer Research Partnership. Common Scientific Outline. https://www.icrpartnership.org/cso.
4Spears PA. 2021. Patient engagement in cancer research from the patient's perspective. Future Oncol. 17(28):3717-3728. doi: 10.2217/fon-2020-1198. Epub 2021 Jul 2. PMID: 34213358.
5Food and Drug Administration. Center for Drug Evaluation and Research (CDER) Patient Focused Drug Development. https://www.fda.gov/drugs/development-approval-process-drugs/cder-patient-focused-drug-development.
Last updated Monday, January 5, 2026
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
