Melanoma



Posted May 22, 2020
Ze'ev Ronai, Ph.D., Sanford Burnham Prebys Medical Discovery Institute, La Jolla
PRCRP FY13 Idea Award with Special Focus, FY17 Expansion Award

Dr. Ze'ev Ronai
Melanoma is the fifth most diagnosed cancer in the United States, with over 96,000 new cases and 7,000 deaths in 2019. Melanoma develops from pigment-producing cells called melanocytes. Most commonly, melanoma occurs on the skin, but can occur in the other areas as well such as the eye (uveal melanoma), mucous membranes (mucosal melanoma), or under nailbeds (acral melanoma). Active duty service members are particularly at risk for developing melanoma due to prolonged periods outside.
The treatment of metastatic melanoma and other cancers experienced a paradigm shift when the FDA approved a new kind of immunotherapy: immune checkpoint inhibitors in 2011 and 2014. Immune checkpoint inhibitors like anti-PD1 and anti-CTLA4 agents work by activating immune cells called T cells. There are multiple types of T cells; in cancer, effector T cells (Teff) function to amplify the anti-tumor response and kill cancer cells. However, the tumor microenvironment is often infiltrated with suppressive immune cells, such as regulatory T cells (Treg), which along with signals from the tumor cells, inhibit the functions of Teff. Anti-PD-1 and anti-CTLA4 block inhibitory signals with the goal of reactivating the anti-tumor T cell responses.
Despite the massive success of immunotherapy, not all melanoma patients respond. A major effort of immunotherapy research focuses on understanding why some patients respond, and some do not. There are many unknowns in the field of immuno-oncology. For example, what factors influence success of checkpoint blockade? Are there any biomarkers that could predict which patients will respond to checkpoint blockade? How can immunotherapy be improved?
Dr. Ze’ev Ronai at Sanford Burnham Prebys Medical Discovery Institute in La Jolla, California, is one of the many scientists trying to answer these questions. He studies a protein called Siah2 that targets the degradation of cellular regulatory proteins and plays a role in cellular response to stress. Dr. Ronai was awarded a Peer Reviewed Cancer Research Program (PRCRP) FY13 Idea Award with Special Focus to study the role of Siah1 and Siah2 in cellular stress signaling in melanoma, followed by a PRCRP FY17 Expansion Award to continue his work studying the role Siah2 plays in melanoma. Recently, results describing the role of Siah2 in anti-tumor immunity were published in the journal Nature Communications.
The results presented from the PRCRP funded research show that when mice are lacking Siah2 (Siah2-/-), melanoma tumor growth is significantly decreased compared to normal mice. Tumors isolated from Siah2-/- mice are significantly smaller with characteristics that reflect an increase in inflammation and immune activation. Further investigation showed that these tumors exhibit increased numbers of Teff cells and a reduction in Treg cells. Loss of Siah2 in Treg prevents these cells from expanding in number and reduced their infiltration to tumors where they antagonize the effect of the Teff cells. With less Treg cells in the tumor microenvironment, Teff cells infiltrate the tumor and can better perform their anti-tumor functions. Siah2-/- mice treated with anti-PD1 antibodies show significant regression in so called “cold” (those that do not respond otherwise to anti-PD1 therapy) melanoma tumor size, compared to untreated Siah2-/- mice or normal mice.
The Cancer Genome Atlas (TCGA) was utilized to assess the clinical relevance of Dr. Ronai’s results. TCGA is a database that has catalogued genetic mutations from over 20,000 primary cancer and matched normal samples in 33 cancer types. Using genome analysis techniques, TCGA has increased understanding of the genetic basis of multiple cancer types. Analysis of 339 metastatic melanoma samples in the TCGA database revealed there is a positive correlation between Siah2 and Treg specific genes, and a negative correlation between Siah2 and genes involved in the anti-tumor Teff response. These findings confirm the clinical significance of a relationship between Siah2 and the anti-tumor T cell responses.
Dr. Ronai’s work therefore suggests that low Siah2 expression could serve as a biomarker to predict which patients will respond to immune checkpoint blockade treatment. Furthermore, strategies to limit Treg numbers or inhibit Siah2 should be explored as potential therapeutic options for patients who do not respond to immune checkpoint blockade monotherapy.
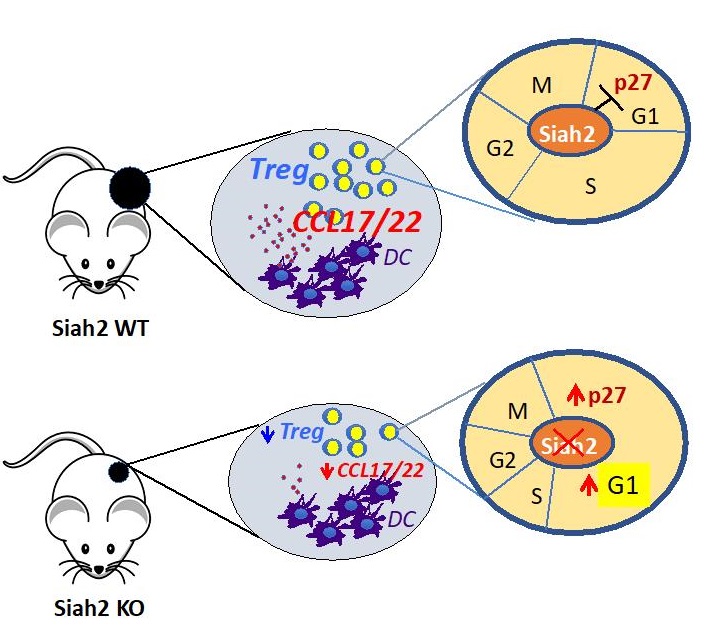
Siah2 KO mice display enhanced anti-tumor immunity that inhibits melanoma growth. This has been achieved by reduced recruitment and proliferation of Tregs which resulted in enhanced anti-tumor immunity. Mechanistically, the absence of the Siah2 gene resulted in elevated expression of p27, a Siah2 substrate, which in turn mediates G1 arrest and reduced proliferation of Tregs. In as much, phenotypes seen in the Siah2 KO resemble those observed following CDK4/6 inhibitors, which are currently in clinical trials. Notably, anti-PD1 therapy of "cold” melanoma-bearing Siah2 KO mice induces complete regression, substantiating the importance of this ubiquitin ligase in immune cell regulation and function. Reduced Siah2 expression coincided with patient response to immunotherapy, pointing to the possible use of Siah2 as a marker for stratification of patients to select therapy.
Reference:
Scortegagna M, Hockemeyer K, Dolgalev I, Poźniak J, Rambow F, Li Y, Feng Y, Tinoco R, Otero DC, Zhang T, Brown K, Bosenberg M, Bradley LM, Marine JC, Aifantis I, Ronai ZA. Siah2 control of T-regulatory cells limits anti-tumor immunity. Nat Commun. 2020 Jan 7;11(1):99. doi: 10.1038/s41467-019-13826-7.
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
