Military Burn
Revised Goniometry for Improved Diagnosis and Physical Therapy for Burn Patients



Posted June 3, 2020
Ingrid Parry, PT, University of California, Davis, and United States Army Institute for Surgical Research

Improvised explosive devices (IEDs) have been used widely against U.S. forces since the early 2000s. IEDs are the leading causes of combat burns and result in a greater Injury Severity Score (ISS), an increase in inhalation injuries, and a larger, full thickness burn size. Future conflicts are projected to involve even more powerful explosive weapons, which may result in a greater number of casualties and more significant injuries including larger and more severe burns. Additionally, these events may occur in areas where medical evacuations may be delayed, potentially for days or even weeks. Burn injuries that may have otherwise been survivable would become life-threatening; and the delayed definitive care will impact mortality and morbidity, including risks for debilitating burn scars. Although the leading causes for civilian burns differ from combat burns, regardless of the causes the majority of severe full thickness burns and tissue injuries often do not heal scar-free. The Military Burn Research Program (MBRP) has invested in research that will provide technologies to prevent or mitigate scar formation at the acute treatment phase, and clinical interventions to reduce debilitating burn scars that have already formed.
In Fiscal Year 2013 (FY13), the MBRP solicited research proposals for the prevention of burn wound contractures and rehabilitation care strategies. One research team noted that in order to address the prevention of burn wound scars, specifically those formed around the joints that often limit the range of motion necessary to execute everyday functions, an accurate method to assess the pathologic scar limitations would be necessary. The research team hypothesized that a more accurate assessment of how the burn scar impacts the burn survivor’s daily function would be important in developing a plan for improved rehabilitation.
The current method to measure a patient’s outcomes in terms of joint range of motion, called goniometry, was established more than 90 years ago and is an accepted clinical and research practice in rehabilitation. However, the basis for this goniometry is founded on an orthopedic model of joint movement where two boney segments articulate around an isolated joint surface. For the burn-injured patient with scar contracture, the range of joint motions may be limited due to restricted pliability of the burn scar(s) since joint movements also involve skin recruitment (Figure 1). Although the application of goniometry has been used on burn patients for determining disability for many years, burn scars near or around the joints can affect the goniometry results based on patient positioning. This means the standard goniometry method may have been misdiagnosing the severity of disability and the functional limitations in burn populations because it fails to take into account the positions involved in functional movements for daily living activities, such as the ability to fully bend the elbow to feed, which may involve shoulder range of motion that differs from the established goniometry method for determining limitations.

Figure 1: Burn patient with scar contractures that limit elbow flexion.
Physical therapists Ingrid Parry at the University of California, Davis (UCD), and Scott Dewey at the U.S. Army Institute of Surgical Research (USAISR) collaborated and recently completed their FY13 MBRP-funded multi-center clinical study that examined the validity of the standard goniometry method for determining functional outcomes for burn patients with scar contractures. The standard goniometry positions joints proximal to the joint range of motion of interest in a manner to place the skin or scar tissue on slack. The study compared standard goniometry to a newly developed revised goniometry paradigm based on cutaneokinematic factors, which takes into account skin recruitment for range of motion. Unlike the standard goniometry, the revised goniometry removes the slack from adjacent joint skin creases similar to what would be needed to accomplish functional tasks. Thus, the major difference between the standard and revised goniometry methods is the position of the adjacent joints or limb segments when goniometry angles are measured (Figure 2).
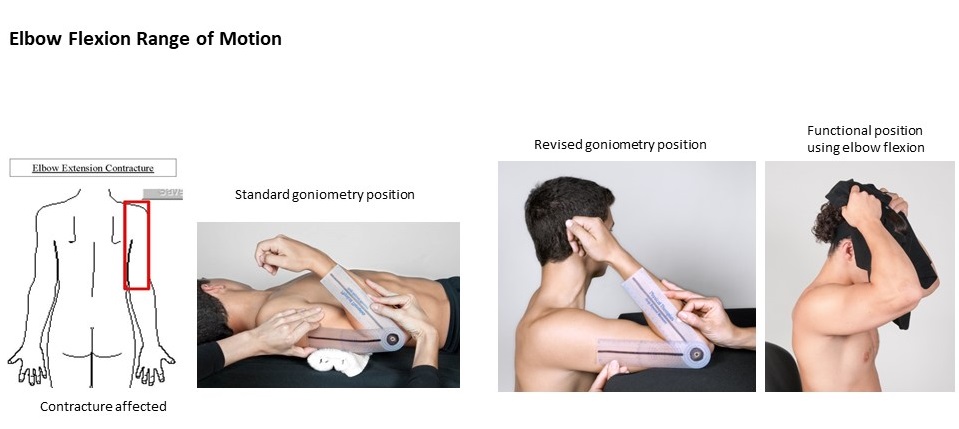
Figure 2: Standard and revised goniometry positioning for measuring elbow flexion range of motion.
The completed prospective multi-center study involved the USAISR as the lead burn center and six additional American Burn Association-certified burn centers. Sixty-six (66) burn patients were enrolled in the study over a period of four years with 1,044 joint position measurements completed using both the revised goniometry and the standard goniometry for comparison. As hypothesized, the revised goniometry, which takes into account the positions impacted by the scar contractures, determined significantly more limitation in joint motion than assessments made using the standard goniometry, 38.8% +/- 15.2% versus 32.1% +/- 13.4% with p<.0001, respectively.
In recognition of outstanding research and the study’s findings, the investigative team lead, Ingrid Parry, received the Andre Zagame Best Rehabilitation Paper Award at the International Society for Burn Injury in December 2018, and the American Burn Association (ABA) Best of Best Abstract and Clinical Research Award at the ABA Annual Meeting in April 2019. The study data was also published in March 2019 in the Journal of Burn Care and Research.*
Given the significance of the findings, investigator Parry also led the development of an app, called “Scar Goniometry,” currently available in the App Store and Google Play for download onto Apple and Android smart devices at no cost, to guide other physical therapists interested in using the revised goniometry method for improving the assessments of functional outcomes for patients with burn scars. To further fully disseminate the research results and the application of the revised goniometry, Ms. Parry and colleague Reg Richard, M.S., PT, have developed a webinar, which will be accessible in the Ameriburn elearn portion of the American Burn Association website (www.ameriburn.org) in May 2020 to help other physical therapists understand the influence of scars on motion and to learn the revised goniometry method and the use of the free app.
Relevant Publications:
*Parry I, Richard R, Aden JK, et al. 2019. Goniometric measurement of burn scar contracture: a paradigm shift challenging the standard. Journal of Burn Care & Research 40(4):377-385.
Parry I, Sen S, Palmieri T, et al. 2019. Current trends in practice for early mobility with the burn population. Journal of Burn Care & Research 40(1):29-33.
Richard R, Parry IS, Santos A, et al. 2017. Burn hand or finger goniometric measurements: Sum of the isolated parts and the composite whole. Journal of Burn Care & Research 38(6):e960-e965.
Ryan CM, Parry I, and Richard R. 2017. Functional outcomes following burn injury. Journal of Burn Care & Research 38(3):e614-e617.
Parry I, Sen S, Sattler-Petrocchi K, et al. 2017. Cutaneous functional units predict shoulder range of motion recovery in children receiving rehabilitation. Journal of Burn Care & Research 38(2):106-111.
Parry I, Forbes L, Lorello D, et al. 2017. Burn rehabilitation therapists competency tool-version 2: An expansion to include long-term rehabilitation and outpatient care. Journal of Burn Care & Research 38(1):e261-e268.
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
