Lupus



Posted August 4, 2020
Laura Plantinga, Ph.D., Emory University

Systemic lupus erythematosus (SLE) is a chronic, heterogeneous autoimmune disease that causes inflammation in numerous tissues within the body. This results in a wide range of symptoms, including significant physical and cognitive functional impairment, decreasing a patient’s ability to carry out the tasks of everyday life. Although assessing and addressing functional impairment is important to patient quality of life, current methods of managing lupus are largely determined by disease activity and other clinical factors (pathogenesis), and are not focused on physical and cognitive function (pathophysiology).
In 2017, Dr. Laura Plantinga of Emory University was awarded a Lupus Research Program Concept Award to improve recognition of and facilitate discussion around the issue of functional impairment in SLE patients. Dr. Plantinga aimed to determine how useful a physical functioning report, possibly including a cognitive assessment, could be to capture, visualize, and quantify functional impairment in an understandable manner for patients and healthcare providers to easily monitor disease progression and develop individualized treatment plans.
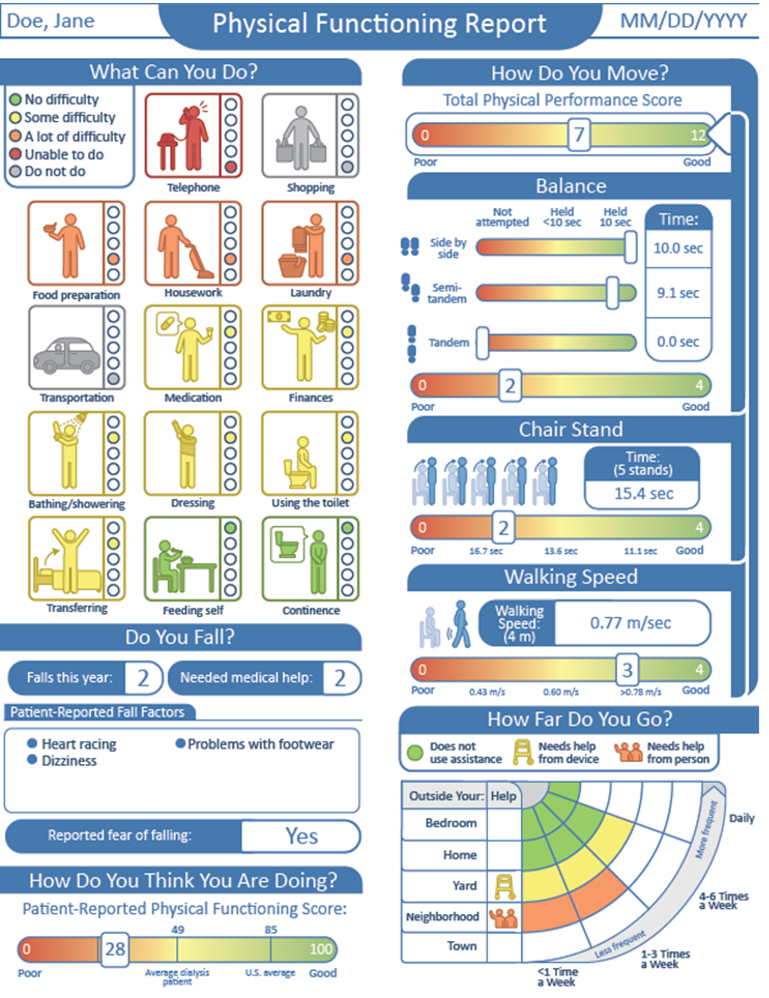
Dr. Plantinga’s team modified an app that was originally developed to create functioning reports for end-stage renal disease so that it was compatible with SLE data. Data from a recent pilot study, in which 60 SLE patients underwent assessments of physical and cognitive functioning, were leveraged to create the app-generated reports. Each report gave the results from self-reports and physician guided exams, included sections rating a patient’s ease of performing everyday activities, their concern for falling, and their mobility including walking speed, balance, and ease of leaving the house via a color and number scale.
Of the patients involved in the leveraged study, 59 of 60 received reports generated by the app, and researchers administered a survey to determine how easy the results were to interpret and how likely patients and healthcare providers were to discuss the results. Ease of interpretation ranged from 70.2% to 85.1%, and 70.2% to 80.5% felt that the report was useful for treatment or care planning. Almost all patients (93.2% to 100%) responded that they would be comfortable discussing the results with a healthcare provider. Interest in receiving a real-time report was reported by 87.2% of patients, and 89.1% expressed a willingness to arrive early to an appointment to receive one.
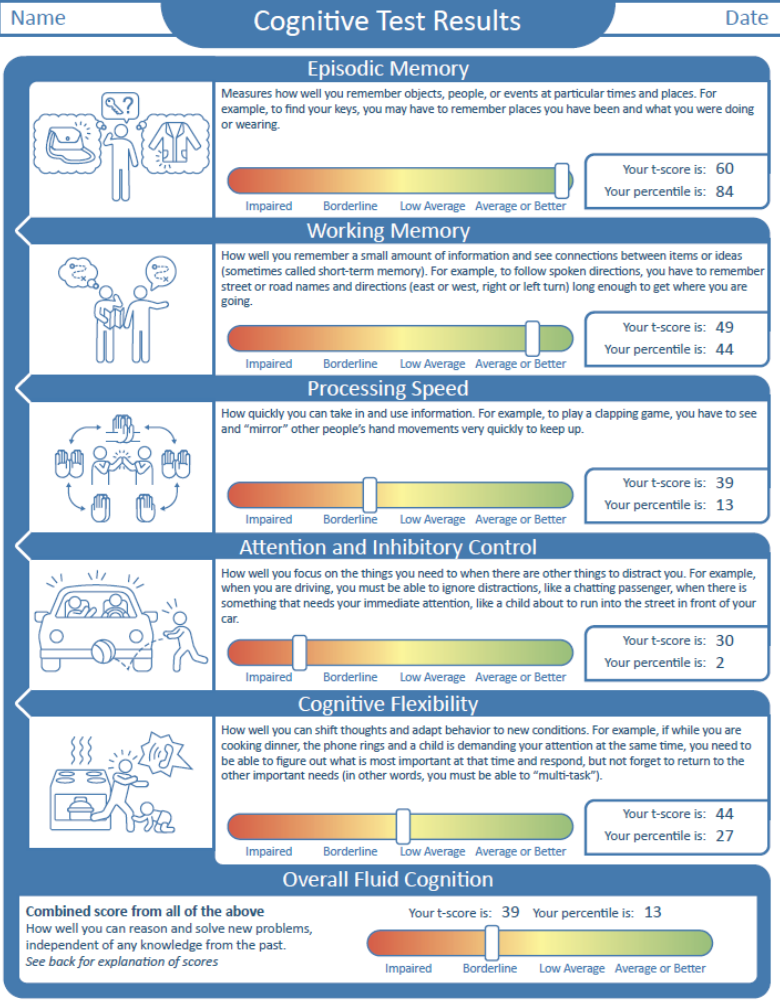
Dr. Plantinga’s team also held two provider focus groups and two patient focus groups. Participants provided feedback on the report and ideas on incorporating cognitive function data. The team is currently analyzing the qualitative data from the focus groups to determine what cognitive performance data would be beneficial for patients and providers to discuss in determining treatment options, and how it should be presented.
Dr. Plantinga’s team continues to complete quantitative analysis of the survey results. They plan to build an app to produce reports for cognitive functioning similar to those created for physical functioning in this study. This app would encourage more studies on clinical implementation of both functioning reports. Use of either or both of these functioning reports could enhance shared decision-making and help us achieve goal-oriented, patient-centered care for those living with lupus.
Link:
Last updated Thursday, November 13, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
