Lung Cancer



Posted July 31, 2020
Kurt Schalper M.D., Ph.D., Yale University

Immune cells use various molecular immune checkpoint systems to recognize normal cells and attack abnormal or foreign cells. One such checkpoint employs a protein-programmed death-ligand 1 (PD-L1) on the surface of normal cells that is recognized by the receptor PD-1 on immune cells. This interaction prevents immune cells from attacking. Cancer cells, although they bear mutations and appear abnormal, can evade immune attack by expressing PD-L1, mimicking normal cells. Immune checkpoint inhibition (ICI) therapies, such as PD-1 blockers, interfere with immune checkpoints like the PD-L1/PD-1 system, allowing immune cells to attack cancer cells. These PD-1 blockers have been found to produce significant and long-lasting remissions, but there are a number of immune checkpoints besides the PD-L1/PD-1 system, and approximately 80% of non-small cell lung cancer (NSCLC) patients still show poor response to PD-1 blockade.
With support from a Fiscal Year 2015 (FY15) Lung Cancer Research Program (LCRP) Career Development Award (CDA), Dr. Kurt Schalper searched for markers capable of predicting the response to ICI in NSCLC patients. Dr. Schalper and his team examined tumor samples collected from NSCLC patients prior to their treatment of PD-1 blockers to differentiate immune cell activity patterns between patients who ultimately responded well to PD-1 blockade (“responders”) from those who did not (“non-responders”). They quantified the numbers of immune cells, measured expression levels of immune-related activation and proliferation molecules in and around the immune cells, sequenced the tumor DNA, recorded the number and types of mutations found, and used computer algorithms to predict the immunogenicity of those mutations (Gettinger, 2018). In addition and using single-cell analysis, Dr. Schalper’s team assessed the levels of immune checkpoint receptors PD-1, Lymphocyte-activation gene 3 (LAG-3), and T-cell immunoglobulin mucin-3 (Tim-3). They found that PD-1 and Tim-3 levels were not predictive of patient response to PD-1 blockers; but non-responders had elevated baseline levels of LAG‑3 in tumor infiltrating lymphocytes, suggesting that upregulation of LAG-3 checkpoint could mediate tumor immune escape when the PD-1 system is blocked (Datar, 2019). Additional work by Dr. Schalper’s team in collaboration with other Yale investigators also characterized a novel LAG-3 receptor ligand called FGL1 that is upregulated in NSCLC patients and participates in tumor-mediated immune evasion (Wang, 2019).
Other researchers reported that tumors from responders contained elevated numbers of mutations, suggesting correspondingly elevated levels of abnormal antigenic peptides that may serve as targets for immune attack. Using a multi-modal approach with high throughput DNA sequencing and immune cell phenotyping, Dr. Schalper's team found that responders' tumors contained elevated numbers of immune cells and that these cells were in a dormant state characterized by a non-exhausted phenotype exhibiting moderate proliferation and cytotoxic immune activity (Gettinger, 2018). Notably, the effect seen was independent of the number of tumor antigenic mutations. These studies proposed that lung malignancies most sensitive to PD-1 axis blockers display a large proportion of lymphocytes that are not terminally differentiated or exhausted; and are therefore capable of reinvigoration with treatment. To test this hypothesis, the team took intact tumor specimens (and the immune cells they contained) from NSCLC patients and transplanted them into immunodeficient mice. They found that treating these mice with checkpoint inhibitors did indeed reinvigorate the tumor immune cells’ activity and produced a favorable anti-tumor immune contexture (Gettinger, 2018). Thus, tumors with a high mutational load containing immune cells lacking an exhausted state (e.g. dormant TILs) represent the optimal environment for immune action that can be stimulated by checkpoint inhibition.
Dr. Schalper’s team also assessed levels of immune-stimulating factors in the blood, since blood collection is a less invasive method of sampling than biopsy collection. In examining patient serum pre- and post-PD-1 blocker treatment, the team found that non-responders tended to have elevated levels of the cytokine interkeukin-8 (IL-8), and IL-8 levels would increase with tumor progression (Sanmamed, 2017). In contrast, responders had lower levels of baseline/pre-treatment IL-8, and those levels further decreased early in treatment (Sanmamed, 2017). Dr. Schalper observed similar patterns in patients with advanced renal cell carcinoma, melanoma, or NSCLC treated with various types or combinations of ICI therapies or other anti-cancer treatments; elevated pretreatment levels of IL-8 predicted poor response to treatment (Schalper, 2020). These results were recently reported in the journal, Nature Medicine (Schalper, 2020), and corroborated and reported in the same journal issue by other researchers. Once standardized and validated, clinical measurements of IL-8 will be developed, and the resultant predictive capability will increase physicians’ ability to build effective treatment plans to optimally benefit cancer patients. Targeting of IL-8 pathway in cases insensitive to PD-1 axis blockers is also envisioned as a future way to treat cancer and a natural extension of Dr. Schalper’s work.
Dr. Schalper received this FY15 LCRP CDA within 5 years of his first faculty position, not having received substantial prior support for lung cancer research. He is now engaged in significant cutting-edge studies and has produced substantial contributions to the field of ICI research. Dr. Schalper was recently awarded the R37 Method to Extend Research In Time (MERIT) Award from the National Cancer Institute (NCI), R37CA245154 entitled “Quantitative and Spatially-Resolved Analysis of the Tumor Immune Contexture for Optimal Diagnosis and Treatment of Lung Cancer.” The NCI MERIT Award is awarded to a small fraction of R01 investigators and allows extension of the project period to seven years. He credits this FY15 LCRP CDA with enabling him to start his laboratory, which has grown to include 12 students and staff working on exciting cancer research projects.
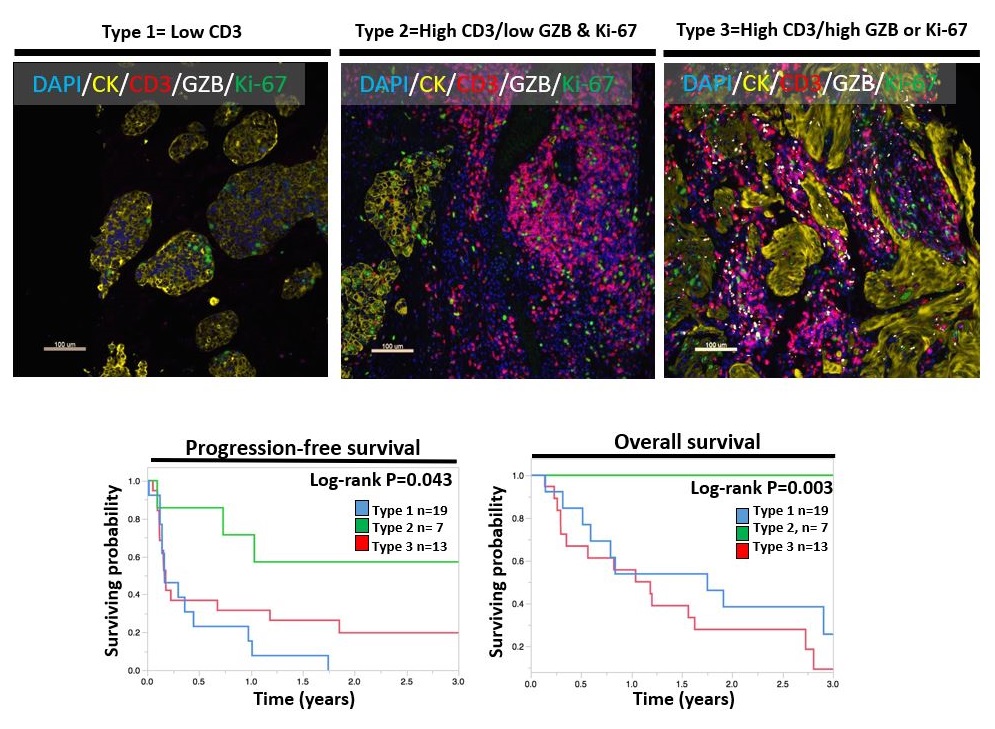
Using reagents that stain different cellular components with different colors, Dr. Schalper's team identified three tumor types. The "Type 2” tumors characterized by lots of immune cells positive for the marker CD3 (red) but with low/moderate proliferation (Ki-67 in green) or immune activity (GZB in white) were found to have the best outcomes after treatment with immune checkpoint inhibitors. The "Type 1” tumors that had low counts of immune cells (red) and "Type 3” tumors that had elevated immune cell counts (red) but with prominent proliferation (green) and immune activity (white) did not benefit as well to treatment. Figure adapted from Gettinger S, Choi J, Mani N, et al. 2018. A Dormant TIL Phenotype Defines Non-Small Cell Lung Carcinomas (NSCLCs) Sensitive to Immune Checkpoint Blockers. Nat Commun 9(1):3196.
Publications:
Datar I, Sanmamed MF, Jun Wang J, et al. 2019. Expression Analysis and Significance of PD-1, LAG-3, and TIM-3 in Human Non-Small Cell Lung Cancer: Using Spatially Resolved and Multiparametric Single-Cell Analysis. Clin Cancer Res 12(15):4663-4673.
Gettinger S, Choi J, Mani N, et al. 2018. A Dormant TIL Phenotype Defines Non-Small Cell Lung Carcinomas (NSCLCs) Sensitive to Immune Checkpoint Blockers. Nat Commun 9(1):3196.
Sanmamed MF, Perez-Gracia JL, Schalper KA, et al. 2017. Changes in Serum Interleukin-8 (IL-8) Levels Reflect and Predict Response to Anti-PD-1 Treatment in Melanoma and Non-Small-Cell Lung Cancer Patients. Ann Oncol 28(8):1988-1995.
Schalper KA, Carleton M, Zhou M, et al. 2020. Elevated Serum Interleukin-8 Is Associated with Enhanced Intratumor Neutrophils and Reduced Clinical Benefit of Immune-Checkpoint Inhibitors. Nat Med 26(5):688-692.
Wang J, Sanmamed MF, Datar I, et al. 2019. Fibrinogen-like Protein 1 Is a Major Immune Inhibitory Ligand of LAG-3. Cell 176(1-2):334-337.e12.
Link:
Last updated Thursday, November 13, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
