Lung Cancer



Posted November 22, 2019
Chengcheng Jin, Ph.D., Massachusetts Institute of Technology

Dr. Chengcheng Jin
Non-small cell lung cancer (NSCLC) is associated with low survival rates and accounts for about 85% of lung cancer cases [1]. The genetic underpinnings that trigger this type of cancer have been widely explored, yet only recently are scientists aiming to understand the role of the lung microbiome in tumorigenesis. Bacterial infections occur in up to 70% of lung cancer patients and can drastically affect clinical outcomes [2]. Although the lungs were once thought to be a sterile environment microbial communities were recently confirmed to exist in the lower respiratory tract, and can even lead to pulmonary disorders such as chronic obstructive pulmonary disease (COPD) and asthma [3]. The mucosal lining of the lungs is exposed to a wide array of foreign bacteria through inhalation, and scientists are now investigating how these diverse groups of bacteria, localized to the mucosal lining of the lung and known as the commensal microbiota, can play a role in tumor initiation and progression.
With support from a fiscal year 2014 (FY14) Lung Cancer Research Program (LCRP) Concept Award, Dr. Chengcheng Jin from Massachusetts Institute of Technology investigated the role of the commensal microbiota of the lung in promoting NSCLC development. To accomplish this, Dr. Jin and her team utilized a mouse model that replicates the two main drivers of human lung adenocarcinoma – point mutations in KRAS and loss of p53 function – to characterize the bacterial composition and abundance of lung microbiota associated with NSCLC. Dr. Jin’s team optimized methods for collecting fluid and tumor tissue from the lungs and then extracted total DNA from the bacterial cells found within the samples. Sequencing analysis was performed to compare the bacterial DNA found in the lungs to that of bacterial DNA found in stool samples, as the gut microbiome is well-defined. The results revealed that distinct bacterial communities existed within the lung compared to the gut. Dr. Jin also discovered that development of lung adenocarcinoma was associated with increased total bacterial burden in the lung and airway tissue, as well as an alteration of the microbiota composition as compared to cancer-free mice.
The results supported by the LCRP award enabled Dr. Jin to further investigate the role of commensal microbiota in regulating tumor initiation and progression in the lung by comparing germ-free mice (mice bred and raised under aseptic conditions, lacking all microorganisms) with conventional mice with normal microbiome. In the germ-free, aseptically raised animals, both tumor burden and number were substantially decreased. Moreover, combined antibiotic treatment with ampicillin, neomycin, metronidazole, and vancomycin resulted in significantly reduced tumor burden in the conventional mice (Figure 1) but failed to inhibit tumor cell growth in vitro, highlighting the critical role that intact commensal microbiota in the lung play in promoting tumorigenesis. This finding also provides strong evidence that manipulation of the microbiota in the lung could lead to new treatment strategies. Currently, Dr. Jin is investigating host immune pathways involved in mediating the effect of the lung microbiome on tumor development. Using flow cytometry, various immune cells associated with lung adenocarcinoma have been characterized, and lung-resident γδ T lymphocytes were found to be particularly important in driving local inflammation and tumor promotion. Thus far, results confirmed that tumor progression is associated with increased bacterial burden and immune activation in the lung.
The results of Dr. Jin’s work, published in Cell [4], indicate that there is a clear link between the local microbiota and lung tumor development, specifically in NSCLC. The FY14 LCRP Concept award funded work that ultimately catapulted further research, providing insights into the role of commensal microbiota in tumor pathogenesis and could lead to new treatment strategies for lung cancer patients through targeting the microbiota of the lung.
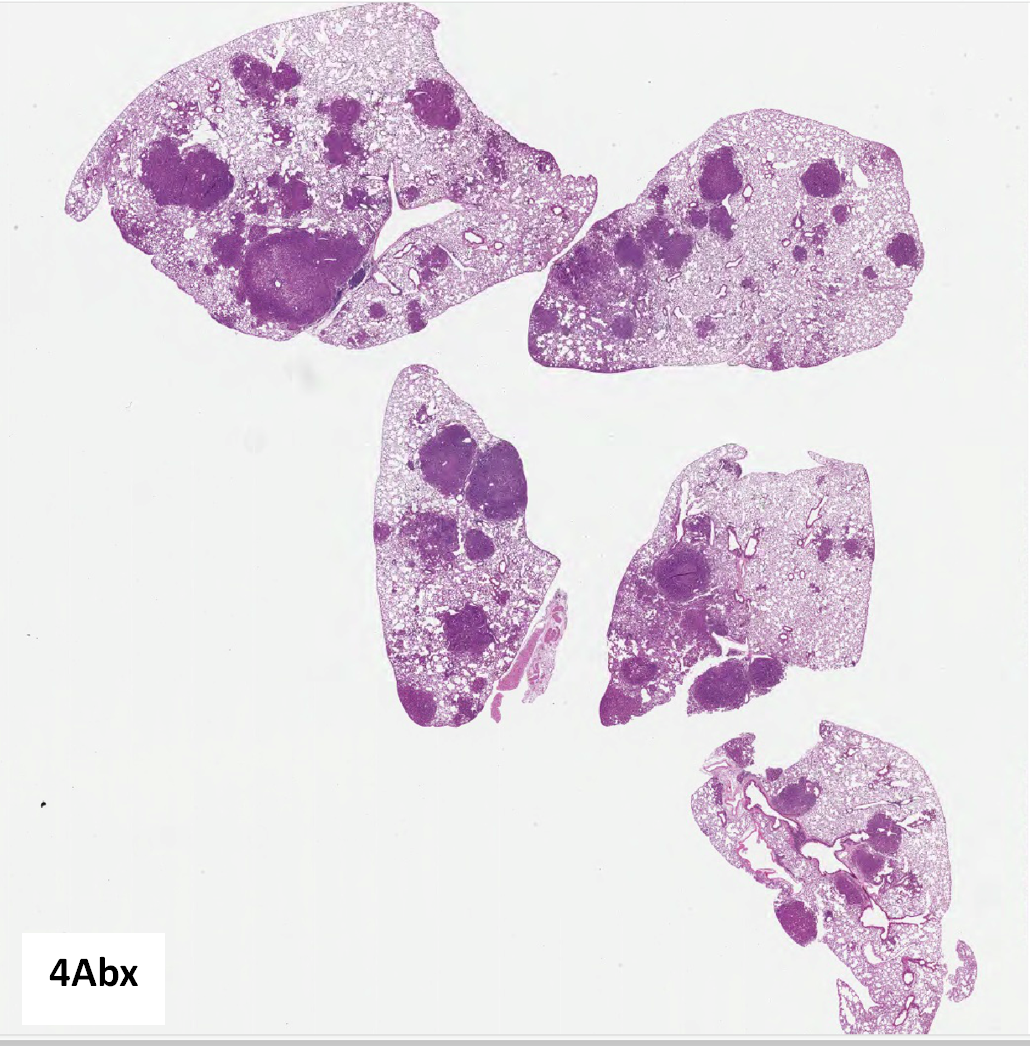
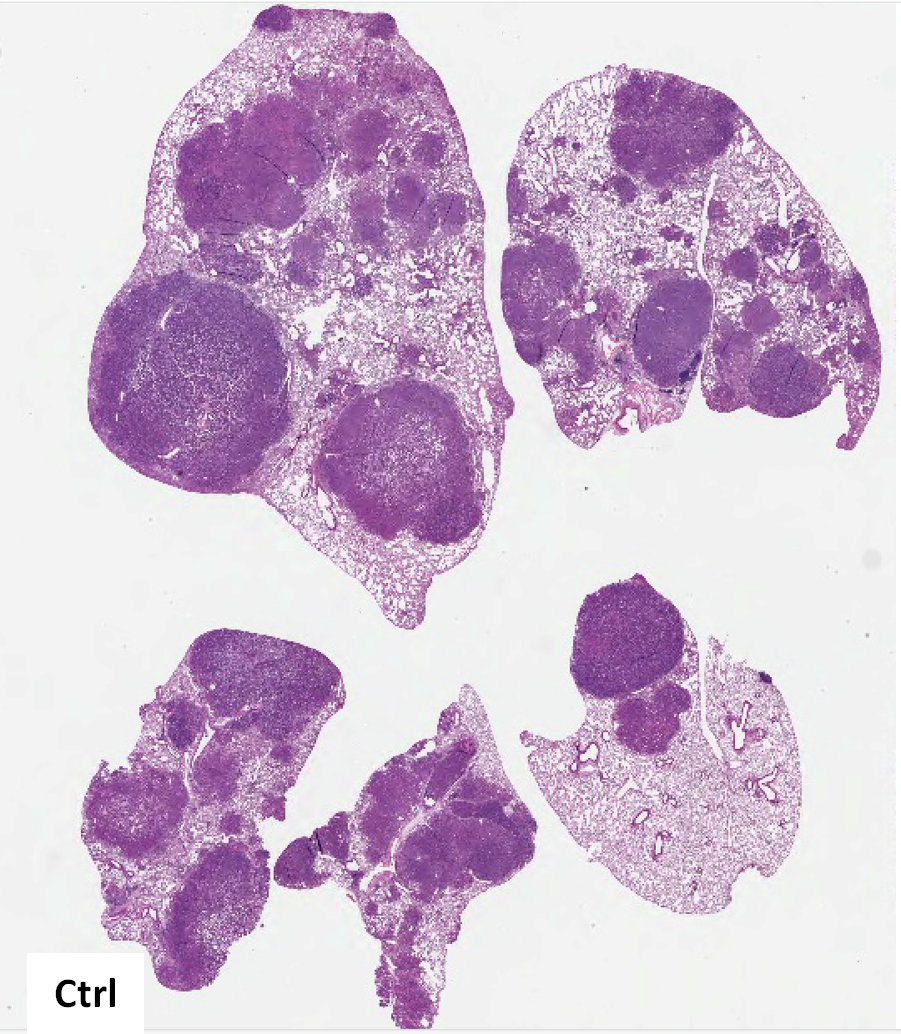
Figure 1. Treatment of specific pathogen-free (SPF) KP mice (GEM model of human LUAD using conditional alleles of Kras LSL-G12D; p53 flox/flox) with combined antibiotics (4Abx) in drinking water starting at 6.5 weeks post-tumor initiation. Tumor burden and grade were analyzed at 15 weeks p.i.
References:
[1] https://www.cancer.org/cancer/lung-cancer.html
[2] Hsu-Kim C, Hoag JB, Cheng GS, and Lund ME. 2013. The Microbiology of Postobstructive Pneumonia in Lung Cancer Patients. J Bronchology Interv Pulmonol. 20(3):266-270.
[3] Dickson RP, Erb-Downward JR, Martinez FJ, and Huffnagle GB. 2016. The Microbiome and Respiratory Tract. Annu Rev Physiol. 78: 481-504.
[4] Jin C, Lagoudas GK, Zhao C, et al. 2019. Commensal Microbiota Promote Lung Cancer Development via γδ T Cells. Cell. 176(5):998-1013.
Link:
Last updated Thursday, December 5, 2024














