Lung Cancer



Posted November 6, 2018
Basil Rigas, M.D., D.Sc., Stony Brook University
Dr. Basil Rigas
Stony Brook University
Stony Brook University
Use of non-steroidal anti-inflammatory drugs (NSAIDs) is thought to be associated with decreased cancer incidence in several cancer types, including lung cancer. (Shebl, Hsing, Park, et al., 2014) However, NSAIDs currently have limited applicability in cancer prevention due to toxicity issues. Sulindac is a chemopreventive NSAID that has been shown to inhibit lung tumor replication by 52% in preclinical animal models, but there is toxicity associated with its long-term use. Phospho-sulindac (PS), a sulindac derivative, was developed with the goal of enhancing the efficacy and improving the toxic effects seen with the parent compound. Preliminary data showed PS to be more effective and less toxic than sulindac in animal models of lung cancer, making it a potential candidate for prevention. The anti-cancer effect of PS was also determined to be driven by reduction oxidation (redox) reactions, which are involved in cell signaling and modulate cell function, including apoptotic cell death. With support from the Department of Defense (DoD), Dr. Rigas and his team at Stony Brook University aimed to further assess the effect of PS in animal models of lung cancer, evaluate the direct delivery of PS to the lungs, and define the mechanism of action of PS against lung cancer.
Dr. Rigas developed a novel delivery system for PS to the lungs using solid lipid nanoparticles (SLNs) - small spherical carriers ranging from 20 to 100 nm in diameter that have shown promise for delivering drug agents. In vitro results showed PS formulation in SLNs (SLN-PS) to be four times more potent than sulindac in multiple lung cancer cell lines. The PI also determined that SLN-PS may directly target mitochondria and disrupt their transmembrane potential, leading to intrinsic apoptosis of lung cancer cells. This was confirmed in subcutaneous tumor xenograft models of lung cancer that showed an accumulation of PS in the mitochondria following SLN-PS treatment, which significantly induced oxidative stress resulting in the destruction of cancer cells. PS-treatment was then evaluated in orthotopic xenograft models of lung cancer, a more clinically relevant model for predicting drug efficacy, which notably showed a 75% reduction in tumor volume.
The PI optimized pulmonary administration of SLN-PS to mice using a novel nose-only exposure system by testing the strength of atomizer, air flow rate, and duration of PS administration. PS was administered at 50 mg/mL for 8 minutes and found to deliver significantly higher levels of the drug to the lungs than aerosol exposure for 2 minutes. Notably, PS-treated mice maintained near-normal lung weight after nose-only exposure and had improved overall survival compared to the vehicle treated group. After 8 weeks, only 6% (1 of 15) of those treated with PS had died compared to 33% (5 of 15) of the mice in the vehicle group.
To further classify the mechanism of action of PS against lung cancer, experiments were performed to define the molecular mechanisms of oxidative stress induced by the agent. In subcutaneous models, oxidative stress led to smaller tumor volume in PS-treated animals. Using orthotopic models, the PI demonstrated that PS suppresses EGFR, an important mediator of cell survival in tumor cells. The research team also found that PS increases reactive oxygen species (ROS) levels, which can sensitize cells to apoptosis and suppress tumor growth. It was determined that the anticancer properties of PS function through its effect on six different mechanisms involved with redox homeostasis, including the activation of NADPH oxidase, an enzyme with the sole function of ROS generation. Taken together, these results indicate that PS induces a redox imbalance that can result in the destruction of lung cancer cells.
This DoD-supported work not only further demonstrated the effectiveness and limited toxicity of PS, but also further characterized its crucial mechanism of action for cancer cell death, making PS a promising candidate for lung cancer prevention. With support from other funding agencies Dr. Rigas and his team are working to further refine the formulation of PS and through a precision medicine approach identify subgroups of patients that will benefit the most from treatment with PS using predictive biomarkers.
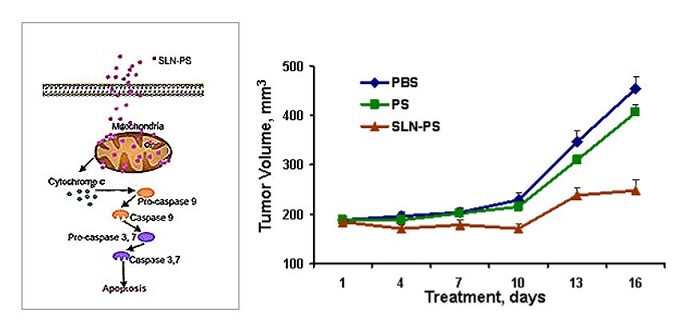
The solid lipid nanoparticles (SLN-PS) direct phosphosulindac (PS) to the mitochondria, inducing massive and selective apoptotic death of the cancer cells (left). The end result is inhibition of the growth of lung cancer xenografts, which is not obtained with unencapsulated phosphosulindac (right).
Publication:
Zhu R, Cheng KW, Mackenzie G, et al. 2012. Phospho-Sulindac (OXT-328) Inhibits the Growth of Human Lung Cancer Xenografts in Mice: Enhanced Efficacy and Mitochondria Targeting by Its Formulation in Solid Lipid Nanoparticles.
Reference:
Shebl FM, Hsing AW, Park Y, Hollenbeck AR, Chu LW, Meyer TE et al. Non- Steroidal Anti-Inflammatory Drugs Use Is Associated with Reduced Risk of Inflammation-Associated Cancers: NIH-AARP Study. PLoS One. 2014. December 31;9(12):e114633 doi: 10.1371/journal.pone.0114633
Last updated Friday, December 13, 2024














