


Posted November 20, 2015
Charles Rudin, M.D. Ph.D., Memorial Sloan Kettering Cancer Center
 Genetic mutations leading to activation of the epidermal growth factor receptor (EGFR) protein are frequently observed in non-small-cell lung cancer (NSCLC) patients. In the past decade, the development and use of tyrosine kinase inhibitor (TKI) drugs that target these mutations have proven to be highly effective treatments for this kind of cancer. Unfortunately, despite initially dramatic responses, TKI resistance eventually develops in most patients. In some cases, the recurrent disease exhibits a histological shift from NSCLC to small-cell lung cancer (SCLC). Due to the retention of EGFR mutations, it is believed these recurrent tumors evolve directly from the initial tumor. With funding from a Fiscal Year 2013 LCRP Idea Development Award, Dr. Charles Rudin is examining the genetic and epigenetic changes that contribute to this shift from NSCLC to SCLC, with hopes of developing better treatment strategies to overcome TKI resistance.
Genetic mutations leading to activation of the epidermal growth factor receptor (EGFR) protein are frequently observed in non-small-cell lung cancer (NSCLC) patients. In the past decade, the development and use of tyrosine kinase inhibitor (TKI) drugs that target these mutations have proven to be highly effective treatments for this kind of cancer. Unfortunately, despite initially dramatic responses, TKI resistance eventually develops in most patients. In some cases, the recurrent disease exhibits a histological shift from NSCLC to small-cell lung cancer (SCLC). Due to the retention of EGFR mutations, it is believed these recurrent tumors evolve directly from the initial tumor. With funding from a Fiscal Year 2013 LCRP Idea Development Award, Dr. Charles Rudin is examining the genetic and epigenetic changes that contribute to this shift from NSCLC to SCLC, with hopes of developing better treatment strategies to overcome TKI resistance.
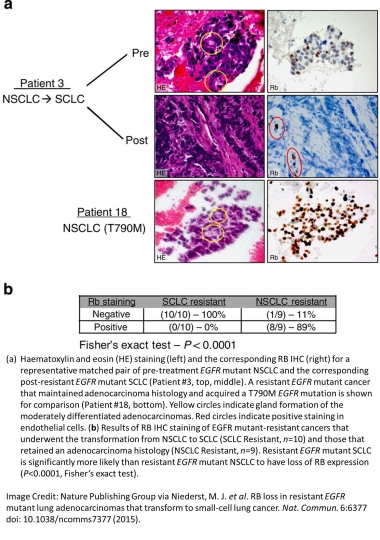
In a study recently published in the journal Nature Communications, Dr. Rudin and colleagues analyzed the molecular changes in TKI-resistant, SCLC-transformed, EGFR mutant tumors from patients. DNA sequencing revealed the presence of genetic mutations specific to these resistant SCLC tumors, including inactivating mutations in the RB1 tumor suppressor gene, which encodes for the retinoblastoma (RB) protein, the inactivation of which is a hallmark of classical SCLC. A loss of RB protein expression was observed universally in a panel of resistant EGFR mutant tumors that transformed to SCLC, but not in those that remained as NSCLC. In further contrast to their TKI-resistant NSCLC counterparts, the SCLC transformed tumors no longer expressed the EGFR protein, despite retaining the EGFR-activating genetic mutation, and exhibited RNA and miRNA expression patterns that more closely resemble classical SCLC. With this in mind, the researchers examined the responsiveness of SCLC transformed tumors to the BCL-2 inhibitor ABT-263 (a therapy currently under examination for the treatment of SCLC), and observed a strong sensitivity, greater than that seen in resistant NSCLC cells or even many classical SCLC cell lines. Notably, however, methylation profiling of SCLC transformed tumors retained a pattern reflected their origins as adenocarcinomas, distinct from primary SCLC.
Together, these results suggest that the subset of TKI-resistant cancers that transform to SCLC acquire some of the key molecular characteristics of classical SCLC, so patients whose tumors undergo this transition could benefit from treatment strategies typically used in this disease. While the identification of a variety of genetic mutations associated with the SCLC transition, including the loss of RB, may improve treatment options, the mechanism of transformation has yet to be fully elucidated. With continuing LCRP support, Dr. Rudin and colleagues plan to answer this question by further examining the genetic and epigenetic changes related to the transformation process. By understanding the mechanism through which lung cancer cells acquire resistance to therapy, better treatments can ultimately be developed to limit recurrence of the disease and improve overall patient outcomes.
Publication:
Niederst MJ, Sequist LV, Poirier JT, Mermel CH, Lockerman EL, Garcia AR, Katayama R, Costa C, Ross KN, Moran T, Howe E, Fulton LE, Mulvey HE, Bernardo LA, Mohamoud F, Miyoshi N, VanderLaan PA, Costa DB, Jänne PA, Borger DR, Ramaswamy S, Shioda T, Iafrate AJ, Getz G, Rudin CM, Mino-Kenudson M, Engelman JA. RB loss in resistant EGFR mutant lung adenocarcinomas that transform to small-cell lung cancer. Nat Commun. 2015 Mar 11;6:6377
Links:














