Kidney Cancer



Posted October 15, 2021
Rupal Bhatt, M.D., Beth Israel Deaconess Medical Center, Boston

Dr. Rupal Bhatt
Immune checkpoint blockade therapy, which controls the activities of T cells, a key cell type in the human immune system, has transformed therapy for cancer patients. Programmed cell death protein 1 (PD1), a protein on the surface of T and B cells, is a checkpoint protein known to help the immune system decide between attacking foreign or abnormal cells and tolerating normal cells, depending on whether PD1 detects PDL1, a ligand for PD-1, on the target cell. Blockade of the PD1 pathway has been an effective cancer immune checkpoint blockade therapy, pushing the immune system to overdrive in attacking cancer cells, even for metastatic renal cell carcinoma (mRCC).1 Unfortunately, many patients do not respond to PD1 immune checkpoint blockade therapy, or develop resistance to this treatment over time,1 thus the need to identify other immune regulatory pathways that work independently of the PD1 pathway.1 HHLA2 is a ligand that interacts with CD28-like receptors on T cells and has been found to be highly expressed in many types of cancer, including RCC.2 HHLA2 can be both costimulatory (promoting immune function) and coinhibitory (inhibiting immune function) on T cells and natural killer (NK) cells.2 Costimulatory effects have been shown to be mediated through the CD28-like receptor TMIGD2, but until recently the coinhibitory CD28-like receptor was unidentified.2 With the help of the Kidney Cancer Research Program (KCRP), Dr. Rupal Bhatt is investigating HHLA2 and its potential as a therapeutic target.
First funded through a Fiscal Year 2017 (FY17) KCRP Concept Award, a collaborative study between Dr. Gordon Freeman’s lab and Dr. Bhatt’s lab, led by principal investigator Dr. Chun-Hau Chen, confirmed that the immunoglobulin-like receptor KIR3DL3 is an inhibitory receptor for HHLA2 in both T cells and NK cells.[1] In addition to confirming the inhibitory receptor, the investigators developed antibodies for HHLA2 and KIR3DL3 that were shown to block the inhibitory action of HHLA2 on immune function, while not affecting the costimulatory signal. The investigators also found that the mechanism by which HHLA2 mediates tumor immune evasion was separate from PDL1, suggesting that blockade of both the PD1 and HHLA2 pathways may be a more effective cancer therapy.
After receiving a follow-on FY20 KCRP Idea Development Award for Established Investigators, Dr. Bhatt and her team plan to expand on this work to identify agents that will effectively block the inhibitory effects of the HHLA2 pathway, to examine the mechanisms of both HHLA2 and the KIR3DL3 receptor, and to gather data to support a phase 1 clinical trial for RCC patients. The first major aim of the study is to identify the mechanisms of KIR3DL3-mediated immune inhibition, including factors that have the potential to increase expression of KIR3DL3 in T cells and NK cells, as well as how KIR3DL3 suppresses T cell and NK cell functions. The team also intends to determine if KIR3DL3 is mediated by immunoreceptor tyrosine-based inhibitor motif (ITIM), and to identify what pathways induce HHLA2 expression. The second major aim of the project is to block HHLA2:KIR3DL3 immune suppression in humanized tumor models. Rodents do not have HHLA or KIR3DL3, so Dr. Bhatt and her team plan to use humanized models to study the immune pathway in vivo and determine if the pathway is an effective therapeutic target in HHLA2-expressing tumors. They will also investigate whether inhibition of the pathway can improve response to PD1 blockade.
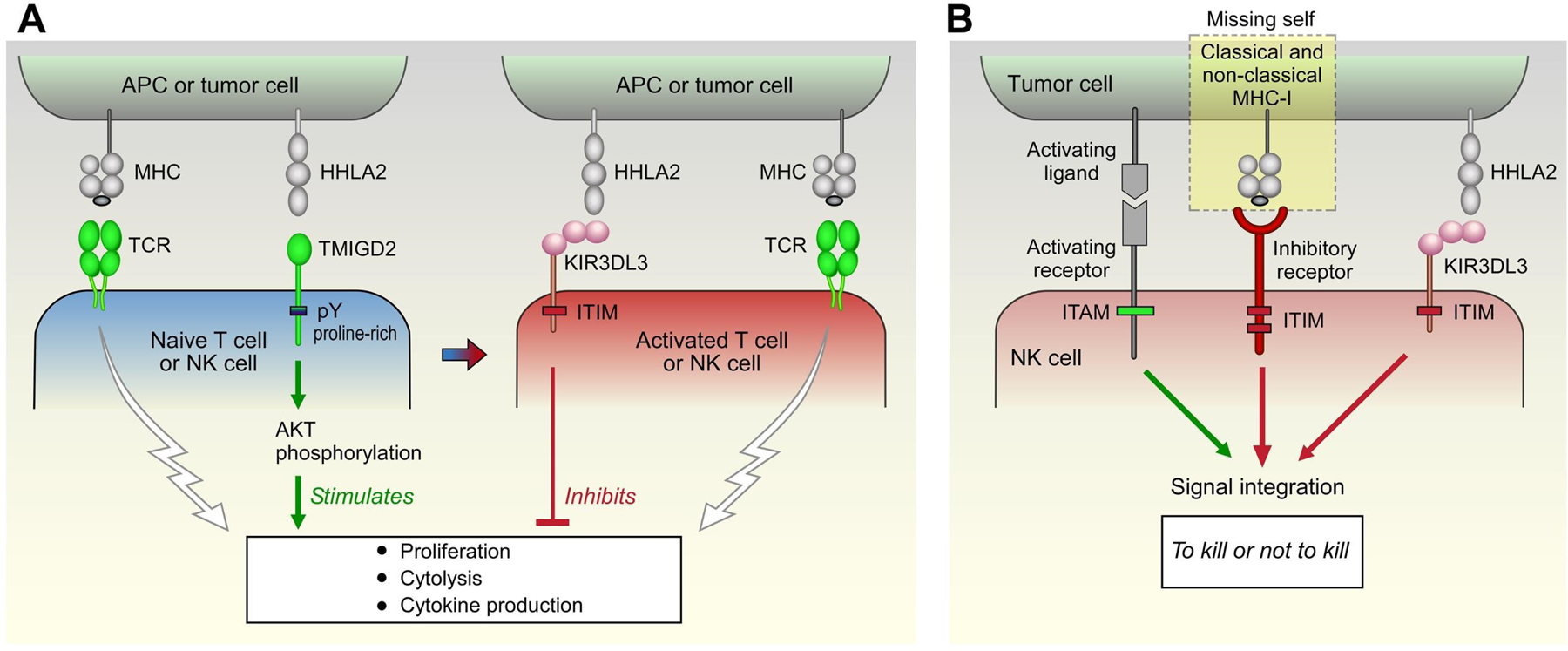
Figure 1: HHLA2 can bind to an immune stimulatory receptor, TMIGD2, or an immune inhibitory receptor, KIR3DL3. The HHLA2 research team led by Dr. Rupal Bhatt is developing strategies to block the inhibitory signal as a new cancer therapy (modified Figure 7 from Bhatt et al., Cancer Immunol Res 2021).
The team aims to leverage the project’s results to launch a phase 1 clinical trial in RCC patients to study the safety and efficacy of the developed antibodies and are partnered with NextPoint Therapeutics to work on pharmaceutical development for their antibody cancer therapy. This study has the potential to provide RCC patients who do not respond to PD1 blockade, or who have developed a resistance to treatment, a new therapy option that could be administered independently, or in conjunction with PD1, to prevent immune evasion by the tumor.

Figure 2: HHLA2 Research Team
References:
1Motzer RJ, Escudier B, McDermott DF, et al. 2015. Nivolumab versus Everolimus in advanced renal-cell carcinoma. NEJM 373:1803-1813.
2Janakiram M, Chinai JM, Zhao A, et al. 2015. HHLA2 and TMIGD2: New immunotherapeutic targets of the B7 and CD28 families. Oncoimmunol 4(8):e1026534.
Publication:
[1] Bhatt RS, Berjis A, Konge JC, et al. 2021. KIR3DL3 is an inhibitory receptor for HHLA2 that mediates an alternative immunoinhibitory pathway to PD1. Cancer Immunol Res 9(2):156-169.Links:
Public and Technical Abstracts: Identification of a New Immune Checkpoint Pathway in RCCPublic and Technical Abstracts: Therapeutic Targeting of the HHLA2/KIR3DL3 Axis as a Novel Immune Checkpoint Pathway in Renal Cancer
Last updated Friday, December 12, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
