Combat Casualty Care (JPC-6)
Human Neural Stem Cells, a New Approach to Restorative Therapy for Severe Traumatic Brain Injury



Posted July 26, 2019
Ross Bullock, Ph.D., University of Miami Miller School of Medicine
Dr. Ross Bullock
Traumatic brain injury (TBI) is a worldwide issue and accounts for nearly half of the injury-induced deaths1. In the urban United States, firearm-related TBI is now the most common TBI mechanism seen in the 25-to-35-year age group2. With increased use of improvised explosive devices, TBI has become a common injury of the Iraq and Afghanistan wars, with 30% of injured Service members returning home with TBI3, 4. Currently, the Department of Defense (DoD) has no effective restorative therapy to prevent the debilitating effects of the most severe type of TBI, penetrative TBI (PTBI) caused by bullet and shrapnel wounds. Although endogenous brain repair occurs after PTBI, it is insufficient to repair neuronal and axonal loss, which lead to significant neurological impairment. Rodent and preclinical studies suggest that use of human neural stem cell transplants can generate new neurons to replace damaged neurons and other neural cells, rebuild injured brain to improve function. In response to a Psychological Health and Traumatic Brain Injury Research Program Broad Agency Announcement released in 2015, Dr. Ross Bullock set out to provide proof-of-concept evidence that transplantation of clinical trial grade human neural stem cells (Neuralstem Inc. NSI-566 cell line) into injured brains following PTBI promotes neural regeneration and functional improvement.
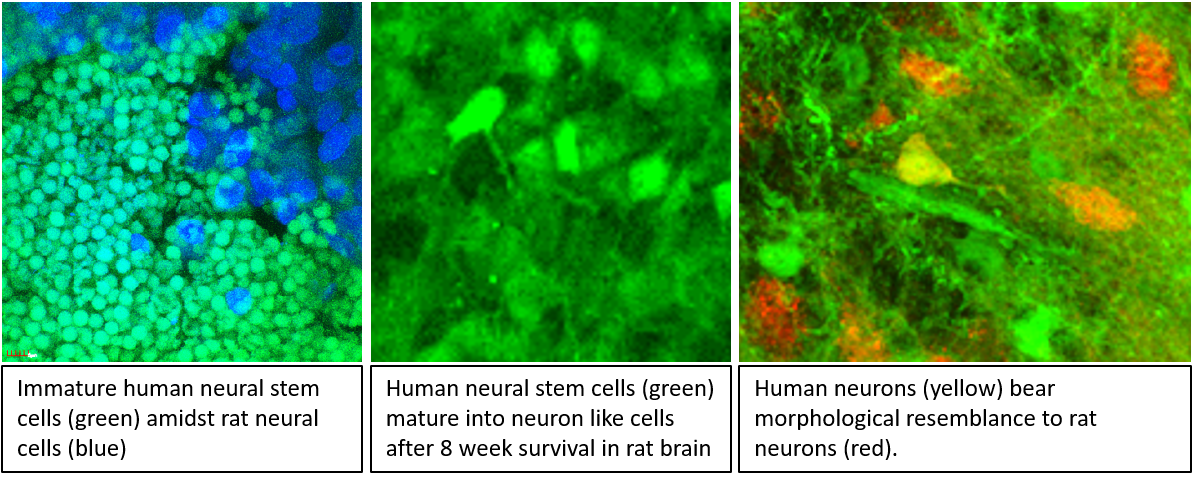
Under this DoD funding opportunity, Dr. Bullock collaborated with Dr Deborah A Shear at Walter Reed Army Institute of Research to study whether transplantation of the NSI-566 cell line PTBI rodent models induces neural regeneration and improve functional outcomes. In a recent paper in the Journal of Neurotrauma5, Dr. Bullock and his team showed that, by 8 weeks post-transplantation, NSI-566 cells had successfully integrated into ~88% of the rats tested. These cells were not only persisted in the rat brains, but also increased in size with neuronal-like processes, producing complex neuronal networks. In animals that survived longer, neuronal differentiation increased among the NSI-566 cells, and they appeared similar to neighboring non-transplanted host neurons. It was clear that the human NSI-566 neural stem cells were able to develop into neurons in injured rat brain; however, the question of whether these neurons were functional and able to contribute to cognitive function so often lost with PTBI remained. To answer this question, Dr. Bullock used the Morris water maze behavioral assessment to evaluate spatial memory in rats with PTBI. It was observed that, at 8 weeks post-transplantation, rats that had received transplanted NSI-566 cells completed the behavioral tests faster than PTBI animals that had not received transplants; thus, evidence of a beneficial effect 8 weeks post-transplantation was concluded.
Having clinically available treatments is of the utmost importance to Service members and patients suffering with TBI. With that in mind, Dr. Bullock and his team reviewed the Food and Drug Administration’s guidelines for the translation of cell transplantation approaches in TBI and are currently working on dose refinement and safety testing for the NSI-566 cells in an effort to further this restorative therapy toward human clinical trials. If successful, Dr. Bullock’s approach could potentially improve quality of life and independence for TBI patients by restoring function to brain areas that were previously injured.
References:
1 Dutton R, Stansbury L, Leone S, et al. 2010. Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns. The Journal of Trauma 69(3): 620-626.
2 Samandouras G. The neurosurgeon’s handbook. Oxford University Press: Oxford; New York, 2010.
3 Okie S. 2005. Traumatic brain injury in the war zone. The New England journal of medicine. 352(20): 2043-2047.
4 Wang E, Huang J. 2013. Understanding and treating blast traumatic brain injury in the combat theater. Neurological research. 35(3): 285-289.
Publication:
5Spurlock M, Ahmed A, Rivera K, Yokobori S, Lee S, Sam P, Shear D, Hefferan, Hazel T, Johe K, Gajavelli S, Tortella F, and Bullock R. 2017. Amelioration of Penetrating Ballistic-Like Brain Injury Induced Cognitive Deficits after Neuronal Differentiation of Transplanted Human Neural Stem Cells. Journal of Neurotrauma 34:191-1995.
Link:
Last updated Thursday, December 5, 2024














