Military Infectious Diseases Research Program (JPC-2)
Next Generation Antimicrobial Wound Dressings to Reduce Infection and Promote Wound Healing



Posted March 1, 2016
Warren Haggard, MSE, Ph.D., University of Memphis
 Musculoskeletal trauma is one of the most common types of injury in the United States. Injuries to the extremities are especially susceptible to serious infection, which can involve drug-resistant bacteria, such as Staphylococcus aureus, and fungi, such as Candida albicans. Invasive fungal infections (IFI) are a particularly significant problem for both the US military (over 78% of injured Soldiers who acquired IFI in Afghanistan between 2009 and 2010 required amputations) and for civilians (Candida is the third most common cause of hospital-acquired infection).
Musculoskeletal trauma is one of the most common types of injury in the United States. Injuries to the extremities are especially susceptible to serious infection, which can involve drug-resistant bacteria, such as Staphylococcus aureus, and fungi, such as Candida albicans. Invasive fungal infections (IFI) are a particularly significant problem for both the US military (over 78% of injured Soldiers who acquired IFI in Afghanistan between 2009 and 2010 required amputations) and for civilians (Candida is the third most common cause of hospital-acquired infection).
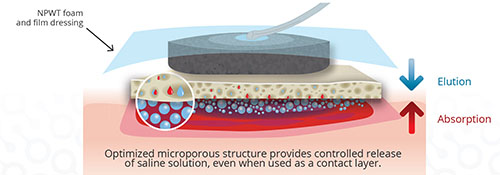
Dr. Warren Haggard at the University of Memphis, with funding support from the Military Infectious Diseases Research Program (MIDRP), is developing a next-generation wound dressing to prevent infection and aid in wound healing for trauma patients. The wound dressing is a naturally sourced biocompatible sponge material and this sponge like wound dressing is a commercially available product from Bionova Medical. Dr. Haggard's team is currently investigating improved versions of the technology with the added functionality to deliver both antibiotic and antifungal agents directly to the wound.
In 2011, Dr. Haggard received a MIDRP Applied Research and Advanced Technology Development Award to develop a biodegradable wound dressing that protects the wound while directly delivering multiple microbe-killing drugs to a contaminated wound. This approach allows high drug concentrations to be delivered locally to treat and prevent infection, while minimizing drug-related side effects by reducing whole body antimicrobial dosing. The sponge can be made from chitosan - a biomaterial made from crustacean shells - or from a blend of chitosan and a biocompatible plastic material that can be found in other drug compositions. Dr. Haggard's team has devised a way to pre-load sponges in the operating room with both the antibacterial drug vancomycin and the antifungal drug amphotericin B. Recent pre-clinical results with the dual loaded sponge delivery system have demonstrated continuous release of therapeutic doses of both drugs directly at the site of injury and prevention of biofilm formation with polymicrobial contamination.
The commercialized sponge, Sentrex BioSponge™, was launched as a wound dressing product in August 2014. Its first use occurred at the John H. Stroger, Jr. Hospital of Cook County (formerly Cook County Hospital) in Chicago, and since then it has been used in over 900 clinical trauma cases at facilities across the country, including military treatment facilities. Used in combination with surgical debridement, irrigation, and systemic antibiotic regimens, this low-cost infection prevention device is already improving treatment outcomes for extremity fractures in civilian patients. With the improvements currently in development, the next-generation sponge is expected to continue to reduce recovery time and lower healthcare costs of these traumatic injuries.
These findings were published in the Journal of Orthopaedic Research (PMID: 25408519), the Journal of Biomedical Materials Research (PMID: 25615516), Macromolecular Bioscience (PMID: 26756211), and registered with the US Patent Office (Patent No. 8,993,540 B2).
Links:
Last updated Thursday, December 5, 2024














