Bone Marrow Failure



Posted October 4, 2017
Matthew Walter, M.D., Washington University

Matthew Walter, M.D.
Washington University
Washington University
Myelodysplastic syndromes (MDS) are a family of disorders in which bone marrow cells display aberrant maturation, resulting in ineffective blood cell production. MDS is the most common myeloid (bone marrow) malignancy in the elderly, and one third of MDS patients will progress to acute myeloid leukemia, an aggressive form of leukemia with a low survival rate. The only curative therapy, bone marrow transplantation, is often not an option due to patient age and comorbidities, so there is an urgent need for better treatment strategies. Over 50% of MDS patients express mutations in splicesosome proteins, which are proteins responsible for the proper RNA splicing and processing that are essential for normal cell functioning. Specifically, mutations in the spliceosome gene U2AF1 occur in 11% of patients with MDS. The mechanisms by which these mutations contribute to MDS are unclear. Dr. Walter aimed to elucidate these mechanisms with support from a fiscal year 2012 Bone Marrow Failure Research Program Idea Development Award.
Dr. Walter created a mouse model to study the most abundant U2AF1 mutation found in MDS patients, which codes for U2AF1(S34F) [1]. Expression of either the wild-type (normal) version of human U2AF1 protein (U2AF1[WT]) or expression of the mutant protein (U2AF1[S34F]) was induced in the bone marrow cells of the mouse. U2AF1(S34F) expression in the mouse model produced a similar pattern of altered splicing to that detected in human MDS samples that express that same mutation. Mice with induced expression of U2AF1(S34) develop characteristics associated with MDS, such as low white blood cell counts and altered bone marrow cell production, yet do not fully develop MDS. Dr. Walter hypothesizes that, in addition to the U2AF1(S34F) mutation, other cooperating mutations are necessary to drive full-blown MDS. Using the U2AF1(S34F) mouse model, Dr. Walter was able to characterize changes in gene expression and RNA splicing induced by U2AF1(S34F) and identified those changes that were also present in MDS patient bone marrow samples. The genes with altered expression or splicing represent candidate genes that may contribute to myeloid disease pathogenesis.
In addition to MDS, splicing alterations are known to be important factors in a number of other diseases, such as cancer. The U2AF1(S34F) mouse model provides a means to explore therapeutic approaches to treating diseases mediated by spliceosome protein mutations. Dr. Walter hypothesized that cells carrying a spliceosome gene mutation would be made more sensitive to further disruption of the spliceosome by splicing modulator drugs, such as sudemycin. Sudemycin treatment in the U2AF1(S34F) mouse model caused increased apoptosis of the U2AF1(S34F)-expressing cell population that displays MDS characteristics and also prevented their expansion [2]. Similar patterns of altered splicing events were detected in both U2AF1(S34F) and U2AF1(WT)-expressing cells treated with sudemycin. However, an additive effect on the splicing pattern induced by both U2AF1(S34F) mutation and drug treatment exceeded the individual effects of mutant U2AF1(S24F) expression or sudemycin treatment alone. These enhanced splicing events, such as increased inclusion or exclusion of gene fragments, or changes in gene expression may result in the increased apoptosis seen in the spliceosome mutant cells. Thus, Dr. Walter's results suggest that the combination of mutant splicing factor expression with a splicing modulator drug like sudemycin may be toxic for the mutant cell and represent a possible therapeutic avenue for MDS patients.
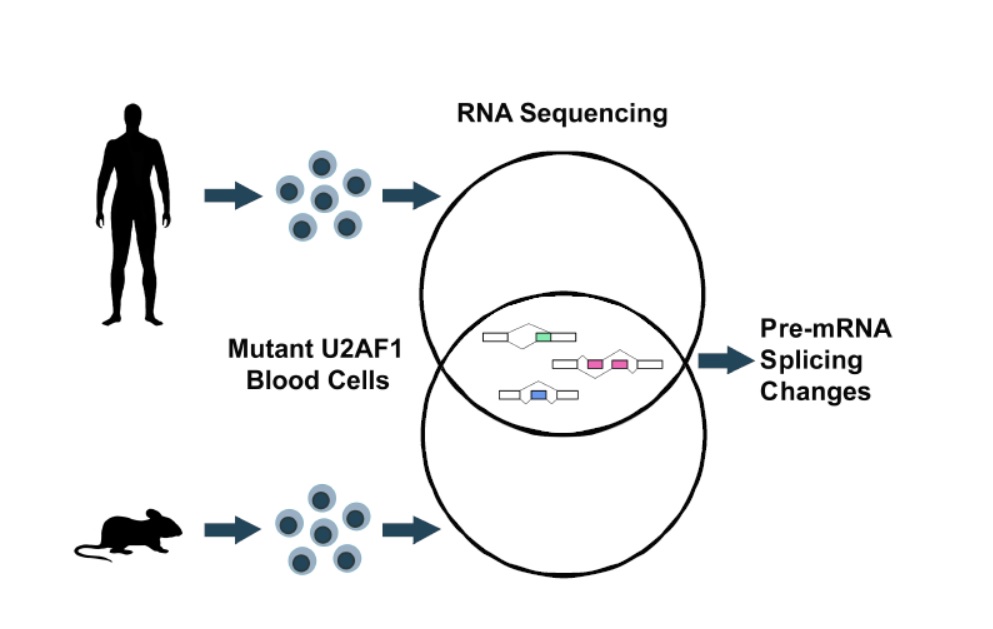
The U2AF1 mutation commonly found in myelodysplastic syndromes alters RNA splicing and gene expression in the U2AF1 mutant mouse model similarly to MDS patients
Publications:
Shirai CL, Ley JN, White BS, Kim S, Tibbitts J, Shao J, Ndonwi M, Wadugu B, Duncavage EJ, Okeyo-Owuor T, Liu T, Griffith M, McGrath S, Magrini V, Fulton RS, Fronick C, O'Laughlin M, Graubert TA, and Walter MJ. 2015. Mutant U2AF1 expression alters hematopoiesis and pre-mRNA splicing in vivo. Cancer Cell. 27(5):631-43.
Shirai CL, White BS, Tripathi M, Tapia R, Ley JN, Ndonwi M, Kim S, Shao J, Carver A, Saez B, Fulton RS, Fronick C, O'Laughlin M, Lagisetti C, Webb TR, Graubert TA, Walter MJ. 2017. Mutant U2AF1-expressing cells are sensitive to pharmacological modulation of the spliceosome. Nat Commun. 8:14060.














