Breast Cancer
New Diagnostic and Therapeutic Approaches to Eradicating Recurrent Breast Cancer



Posted October 16, 2020
Sandra McAllister, Ph.D., Brigham and Women's Hospital

Triple-negative breast cancer (TNBC), an aggressive subtype of breast cancer, affects women of all ages equally, representing 10%-15% of breast cancer incidence across all age groups. Immune checkpoint blockade (ICB) therapy, which has shown clinical success for the treatment of other cancers, recently gained interest as a treatment for TNBC. Several U.S. Food and Drug Administration-approved antibody-based ICB therapeutics target key regulators of the immune system (e.g., immune checkpoint molecules), resulting in immune response activation and subsequent destruction of tumor cells via T cell-mediated immunity. However, age-related changes to immunity, such as decreased ability to activate T cell lymphocytes, is well documented and could present challenges to the efficacy of immunotherapy in breast cancer. Moreover, older patients are typically excluded from or underrepresented in trials evaluating ICB in TNBC. As a result, the impact of age-related immune dysfunction on the response to ICB therapy remains unknown. With funding from a Fiscal Year 2013 Breast Cancer Research Program Era of Hope Scholar Award, Dr. Sandra McAllister sought to define age- and ICB-related changes to the TNBC tumor microenvironment and determine whether aged immune phenotypes affect the efficacy of ICB therapy for the treatment of TNBC.
As reported in a recently published article in Cancer Discovery, Dr. McAllister and her team used mouse models of TNBC to evaluate whether the age-dependent changes to T cell immunity influence the response to ICB therapy, specifically the response to therapeutics targeting either programmed death-ligand 1 (PD-L1) or cytotoxic T-lymphocyte-associated antigen 4 (CTL4A) immune checkpoint proteins. Following treatment with either anti-PD-L1 or anti-CTLA4, young tumor-bearing mice exhibited significantly decreased tumor growth and increased overall survival, whereas ICB treatment only marginally slowed tumor growth or had no effect on the tumors of aged mice. Importantly, tumors from aged mice exhibited an increased emergence of an immunologically “cold” tumor microenvironment, characterized by absence of tumor infiltrating lymphocytes and decreased signaling of antitumor signaling pathways, including interferon-gamma (IFN-gamma), IFN-alpha, and other inflammatory responses.
Intratumoral expression of IFN pathway genes is closely associated with response to ICB. Dr. McAllister and her team noted that control tumors (i.e., without ICB therapy) from young mice were enriched for antitumor gene sets compared to tumors from aged mice, indicating that age-dependent differences in the baseline expression of IFN-related genes were evident prior to treatment. Consistent with preclinical observations, TNBC samples from the Molecular Taxonomy of Breast Cancer International Consortium genomic database exhibited enriched antitumor responses and increased levels of active T cells in patients ≤40 years of age relative to those ≥65 years of age. Taken together, these results suggest that tumor genomic data may provide prognostic utility for patients selected to receive ICB therapy.
Dr. McAllister’s lab next explored whether stimulation of IFN signaling with the IFN pathway agonist DMXAA (5,6-dimethylxanthenone-4-acetic acid), would be sufficient to trigger response to ICB in aged mice. While ICB and DMXAA were ineffective in improving survival of aged mice when administered alone, DMXAA + ICB combination therapy significantly reduced tumor growth, resulting in improved overall survival. Importantly, the addition of DMXAA to ICB therapy did not enhance outcomes for young mice.
This research presents a breakthrough in understanding how age-related changes to peripheral immunity and the tumor microenvironment influence the efficacy of ICB therapy for the treatment of TNBC. These findings provide evidence for leveraging IFN-related tumor genomic data as a prognostic indicator of response to ICB mono- or combination therapy. Importantly, the results of this project suggest that ICB coupled with IFN pathway agonists can activate T cell responses within the immunologically “cold” tumor microenvironment commonly observed in older TNBC patients, thus identifying a new potential treatment regimen. Dr. McAllister received a Fiscal Year 2019 Expansion Award from the Breast Cancer Research Program, enabling her to further evaluate the efficacy of ICB combined with IFN pathway agonists for the treatment of TNBC in older patients.
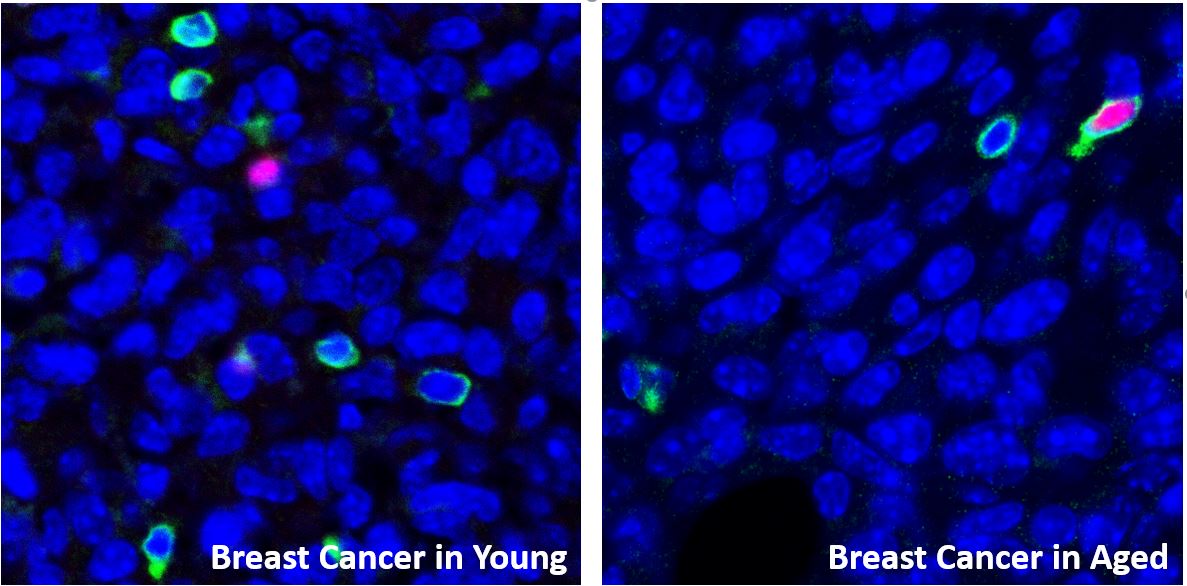
Old Stay Cold. Triple-negative breast cancer (TNBC) tumors in young mice (left) show signs of an activated “hot” immune system while the TNBC tumors in aged mice (right) have an attenuated “cold” immune response. After treatment with immune checkpoint blockade therapy, the immune response in the tumors of young mice becomes even more active while the immune response in tumors from aged mice stays cold. In the images, cells that are exclusively blue are TNBC tumor cells (DAPI+), cells that are both green and blue are T lymphocytes (CD3+), and cells that are labeled both green and pink are T-regulatory cells (Foxp3+/CD3).
Publication:
Sceneay J, Goreczny GJ, Wilson K, et al. 2019. Interferon signaling is diminished with age and is associated with immune checkpoint blockade efficacy in triple-negative breast cancer. Cancer Discovery 9(9):1208-1227.
Link:
Last updated Thursday, November 13, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
