Breast Cancer
Targeting the Cytoskeletal Physics of Circulating Breast Tumor Cells to Reduce Metastasis



Posted April 24, 2018
Stuart S. Martin, Ph.D., University of Maryland, Baltimore (UMB)
Greenebaum Comprehensive Cancer Center

Dr. Stuart S. Martin
Circulating tumor cells (CTCs) are an established indicator of long-term prognosis and metastatic risk in breast cancer (BC) patients.1 Dramatic increases in the number of CTCs can be detected in BC patients following surgery and neoadjuvant chemotherapy. Such increases can even be detected in patients with tumor-free margins, leading to an increased metastatic and relapse risk, as well as decreased patient survival.2,3 The lack of technologies capable of isolating CTCs for study has been a major barrier to understanding CTC biology. Current technologies include placing CTCs on an adherent surface rather than in a free-floating environment similar to that which CTCs experience in the blood stream during metastasis. Not allowing the technology shortfalls to discourage him, Dr. Stuart Martin proceeded to study CTCs, hoping to further the field's understanding of these metastatic cells. As a result of his work, Dr. Martin discovered that detached BC cells form a new tubulin-based cancer cell appendage, termed microtentacles.4 Microtentacles have been shown to be enriched in the CTC population and to promote metastasis of CTCs through the reattachment of BC cells to each other and to endothelial layers,5,6 as well as increasing CTC retention in the lung.7
With support from a Fiscal Year 2010 Breast Cancer Research Program Era of Hope Scholar Award, Dr. Martin focused on the development of technologies able to rapidly isolate live CTCs so that CTC biology, specifically microtentacles, and their response to drugs could be studied. Using microfluidic cell tethering technologies, Dr. Martin, in collaboration with Dr. Christopher Jewell's bioengineering group at the University of Maryland, College Park, developed a strategy to capture and study CTCs in a non-adherent microenvironment. The microfluidic cell tethering technology they developed utilizes nanoscale polyelectrolyte multilayers (PEMs) composed of polymethacrylic acid and polyacrylamide to prevent BC cell binding. A hydrophobic lipid was then incorporated into the upper PEM layer to facilitate binding and capture of CTCs, securing the cells and preventing drift. The new microfluidic cell tethering technology allowed for high-resolution images of the tethered cells to be obtained in real time. In a recent Oncotarget publication, Dr. Martin and his team showed that both MDA-MB-436 and MCF-7 BC cell lines were able to bind to the lipid-coated device surface while preserving non-adherent tumor cell behaviors, like microtentacles, and while having no negative impact on tumor cell viability. Importantly, this technology reduced the blurring of images, which allowed the team to develop an automated analysis of microtentacles behavior in response to drug treatment. Using the automated analysis platform, the team is able to quantitate the number of microtentacles per cell, average microtentacles length, and changes to microtentacles length that occur with various drug treatments. In BC cell lines treated with and without colchicine, a microtubule destabilizing agent, a stark reduction in the number and length of microtentacles was observed.
In addition to developing technologies for experimental use, Dr. Martin and his team sought to develop a clinical technology capable of isolating live CTCs from patient blood samples. Currently, the only FDA-approved method for detecting CTCs in patient samples utilizes the immunomagnetic-based separation CellSearch method. CellSearch utilizes antibodies to the epithelial cell adhesion molecule (EpCAM) attached to magnetic nanoparticles in order to pull CTCs out of patient blood samples. Concerns have been raised that this method misses many CTCs within circulation because it is too restrictive and does not take into consideration the heterogeneity of CTCs. Additionally, this method is time-consuming and relies on chemical fixation of cells, preventing any analyses from being conducted on live CTCs. Therefore, improved detection technology must be developed so that CTCs can be rapidly isolated from patient blood samples and assayed to improve diagnosis, predict metastatic risk, inform treatment, and monitor treatment responses. In collaboration with the nanotechnology company Creatv Microtech, Inc., a microfiltration approach called CellSieveTM was developed, which utilizes wafer photolithography to generate precise pore sizes on a membrane. CellSieveTM allows patient blood to rapidly flow through the CellSieveTM filter, efficiently trapping CTCs while allowing red and white blood cells to pass through. Initial validation studies were performed and recently published in Cytometry A and Royal Society of Chemistry Advances. Using cancer cell line spiked whole peripheral blood, CellSieveTM successfully captured CTCs, and the results were confirmed using duplicate blood samples obtained from BC and prostate cancer patients. In comparative studies, CellSieveTM was found to be superior to CellSearchTM. It recovered CTCs from 72% of patient samples, compared to 52% recovered with CellSearch. CellSieveTM has additional benefits; for instance, this method does not require chemical fixation of cells and allows for a more detailed imaging of live CTCs. Moreover, using CellSieveTM, Dr. Martin and his team identified a novel circulating cancer-associated macrophage-like cell (CAML) that was found to be present in the blood of cancer patients. Preliminary data suggest that the presence of CAMLs could differentiate patients with malignant and benign disease from those without disease, as no CAMLs were detected in blood samples from healthy patient controls (results published in Proceedings of the National Academy of Sciences USA and Cancer Epidemiology, Biomarkers & Prevention).
Currently, little is known about the biology of CTCs and how they respond to treatment. The development of new microfluidic cell tethering technology and CTC isolation methods now provides an integrated platform for scientists to both test anti-metastatic therapies and rapidly characterize patient tumor cells for metastatic potential and drug response. Since study initiation, Dr. Martin's work has resulted in 22 publications, 4 patents, and 36 invited national and international research talks. Two of the patents were issued for the microfluidic cell tethering device. UMB has licensed both of these patents to a startup company, Cellth Systems. The collaboration between Dr. Martin and Cellth Systems was recently funded through the state of Maryland to further develop the tethering technology (TEDCO - Maryland Innovation Initiative, July 2017).
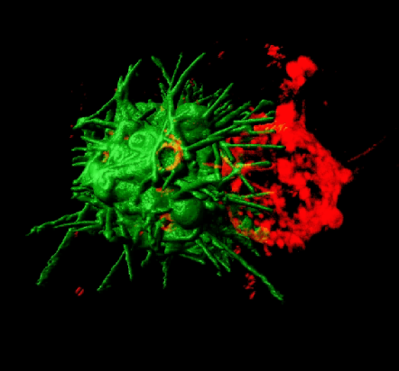
Microtentacles promote clustering of nonadherent tumor cells - CTC clusters have 50x higher metastatic potential.
Matrone, M.A., Whipple, R.A., Balzer, E.M., Martin, S.S. (2010). Microtentacles tip the balance of cytoskeletal forces in circulating tumor cells. Cancer Research 70(20):7737-41.
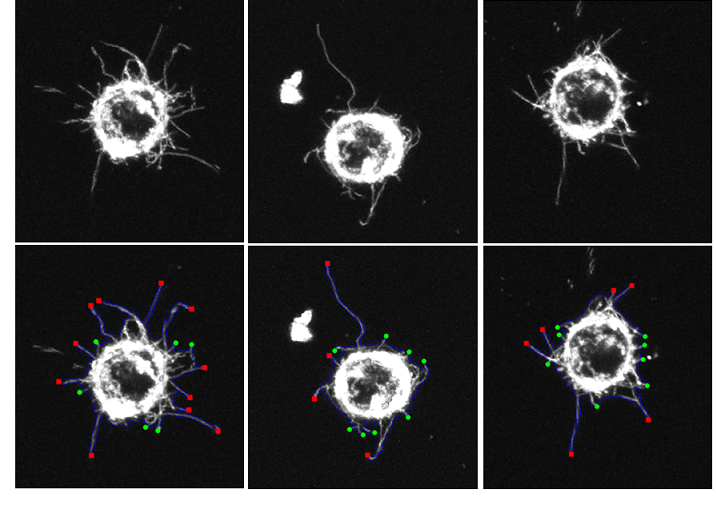 Microtentacles in patient-derived xenograft (PDX) cells
Microtentacles in patient-derived xenograft (PDX) cells
Selected Publications:
Chakrabarti KR, Andorko JI, Whipple RA, Zhang P, Sooklal EL, Martin SS, and Jewell CM. 2016. Lipid tethering of breast tumor cells enables real-time imaging of free-floating cell dynamics and drug response. Oncotarget 7(9):10486-10497.
Adams DL, Adams DK, Alpaugh RK, Cristofanilli M, Martin SS, Chumsri S, Tang CM, and Marks JR. 2016. Circulating cancer associated macrophage-like cells differentiate malignant breast cancer and benign breast conditions. Cancer Epidemiol Biomarkers Prev 25(7):1037-1042.
Adams DL, Martin SS, Alpaugh RK, Charpentier M, Tsai S, Bergan RC, Ogden IM, Catalona W, Chumsri, S, Tang CM, and Cristofanilli M. 2014. Circulating giant macrophages as a potential biomarker of solid tumors. Proc Natl Acad Sci USA 111(9):3514-3519.
Charpentier, M.S., Whipple, R.A., Vitolo, M.I., Boggs, A.E., Slovic, J., Thompson, K.N., Bhandary, L., Martin, S.S. (2014) Curcumin targets breast cancer stem-like cells with microtentacles that persist in mammospheres and promote reattachment. Cancer Research 74(4):1250-60.
Boggs, A.E., Vitolo, M.I., Whipple, R.A., Charpentier, M.S., Goloubeva, O.G., Ioffe, O.B., Tuttle, K.C., Slovic, J., Lu, Y., Mills, G.B., Martin, S.S. (2015). a-tubulin acetylation elevated in metastatic and basallike breast cancer cells promotes microtentacle formation, adhesion and invasive migration. Cancer Research 75(1):203-15.
Vitolo. M.I., Boggs, A.E., Whipple, R.A., Yoon, J.R., Thompson, K., Matrone, M.A., Cho, E.H., Balzer, E.M., Martin, S.S. (2013). Loss of PTEN induces microtentacles through PI3K-independent activation of cofilin. Oncogene 32(17):2200-10.
Kiessling, T.R., Herrera, M., Nnetu, K.D., Balzer, E.M., Girvan, M., Fritsch, A., Martin, S.S., Kaes, J., Losert, W. (2013) Ref.: Ms. No. EBJO-D-12-00135R1 Analysis of Multiple Physical Parameters for Mechanical Phenotyping of Living Cells. Eur. Biophy. J. 42(5):383-94.
References:
1 Jansson S, Bendahl PO, Larsson AM, Aaltonen KE, and Rydon L. 2016. Prognostic impact of circulating tumor cell apoptosis and clusters in serial blood samples from patients with metastatic breast cancer in a prospective observational cohort. BMC Cancer 16:433.
2 Camara O, Kavallaris A, Noschel H, Rengsberger M, Jorke C, and Pachmann K. 2006. Seeding of epithelial cells into circulation during surgery for breast cancer: The fate of malignant and benign mobilized cells. World J Surg Oncol 4:67.
3 Pachmann K, Camara O, Kavallaris A, Krauspe S, Malarski N, Gajda M, Kroll T, Jorke C, Hammer U, Altendorf-Hofmann A, Rabenstein C, Pachmann U, Runnebaum I, and Hoffken K. 2008. Monitoring the response of circulating epithelial tumor cells to adjuvant chemotherapy in breast cancer allows detection of patients at risk of early relapse. J Clin Oncol 26:1208-1215.
4 Whipple RA, Balzer EM, Cho EH, Matrone MA, Yoon JR, and Martin SS. 2008. Vimentin filaments support extension of tubulin-based microtentacles in detached breast tumor cells. Cancer Research 68:5678-5688.
5 Whipple RA, Cheung AM, and Martin SS. 2007. Detyrosinated microtubule protrusions in suspended mammary epithelial cells promote reattachment. Exp Cell Res 313:1326-1336.
6 Balzer EM, Whipple RA, Cho EH, Matrone MA, and Martin SS. 2009. Antimitotic chemotherapeutics promote adhesive responses in detached and circulating tumor cells. Breast Cancer Res Treat 121(1):65-78.
7 Matrone MA, Cho EH, Vitolo MI, Whipple RA, Balzer EM, Yoon JR, Ioffe OB, Tuttle KC, Tan M, and Martin SS. 2010. Metastatic breast tumors express increased tau, which promotes microtentacle formation and the reattachment of detached breast tumor cells. Oncogene 29(22):3217-3227.
Link:
Last updated Wednesday, March 12, 2025














