Breast Cancer
Uncovering a New Pathway to Target and Treat Breast Cancer Metastasis



Posted November 24, 2017
Andy Minn, M.D., Ph.D., University of Pennsylvania

Andy Minn, M.D., Ph.D.,
University of Pennsylvania
University of Pennsylvania
Metastasis, the spread of cancer from the site of the primary tumor to distant organs, is the leading cause of breast cancer-associated deaths and is considered incurable. Once breast cancer metastasizes, tumors become resistant to treatment, even if the primary tumor initially responded. Research has focused on elucidating the mechanisms that mediate treatment resistance in hopes of finding therapeutically targetable pathways to help reduce the mortality associated with metastatic disease. Scientists have demonstrated that the stroma, i.e., the tissue surrounding tumors, is able to "communicate" with cancer cells, resulting in the generation of signals that promote cancer progression and therapy resistance. Exploring the pathways activated by stromal cells surrounding breast tumors would further improve our understanding of the mechanisms mediating treatment resistance and help provide new therapeutic targets.
Dr. Andy Minn from the University of Pennsylvania has dedicated his career to challenging the notion that metastatic breast cancer is incurable. Through studying the interaction between stroma and breast cancer to elucidate pathways that mediate treatment resistance, his work focused on a set of interferon-stimulated genes (ISGs), which can predict how a patient will respond to chemotherapy and radiation treatments. ISGs are normally induced in response to viruses to help the body mount an anti-viral immune response. However, in breast cancer, these ISGs are induced upon contact with stromal cells, and instead of inducing anti-viral immunity, breast tumors expressing ISGs have increased resistance to chemotherapy and radiation. Moreover, ISGs are enriched in tumors from patients diagnosed with triple negative breast cancer, the subtype for which no targeted therapeutics are currently available.
To elucidate why and how stromal cells induce anti-viral genes in breast cancer, whether the activated pathways could serve as clinical biomarkers, and whether these pathways could be therapeutically targeted to restore sensitivity to chemotherapy and radiation treatments, Dr. Minn applied for and was awarded a Fiscal Year 2008 (FY08) Era of Hope Scholar Award and an FY13 Breakthrough Funding Level 2 Award, both through the Breast Cancer Research Program (BCRP).
A summary of Dr. Minn's research over the last nine years conducted under these two BCRP awards was published in two articles in the journal Cell. Using cell culture methods in which ISG-expressing cancer cells are grown with stromal cells (co-culture), the research team discovered that stromal cells released and transferred exosomes to the cancer cells. Exosomes are small vesicles released by cells to communicate with neighboring cells and share several properties with viruses, providing insight into why breast cancer cells mount an anti-viral response upon their transfer. These exosomes were found to contain RNA (exoRNA); specifically, an abundance of non-coding RNA. Non-coding RNA refers to any RNA within a cell that is not used to make a protein; rather, these RNA molecules perform a myriad of other cellular functions including, but not limited to, regulating signaling pathways within cells. Dr. Minn's group identified that a non-coding RNA called RN7SL1 was the exoRNA responsible for the ability of stromal-derived exosomes to mimic viruses, activate cytoplasmic RNA receptors in breast cancer cells, and induce ISGs. Once activated, this anti-viral signaling promotes tumor growth, metastasis, and treatment resistance. Importantly, blocking key parts of this signaling cascade in animal models of breast cancer using targeted therapies can markedly improve response to therapy.
Dr. Minn provided clinical relevance to the cell culture and mouse work. His team co-cultured triple-negative breast cancer cells with a panel of stromal cells isolated from patients' breast tumors following surgical resection. Results from genetic analyses confirmed the patient stromal cells were able to activate pro-tumorigenic and ISG signaling pathways within the breast cancer cells. Moreover, harvesting exosomes from the serum of breast cancer patients demonstrated high levels of RN7SL1 in patients with triple-negative tumors.
Results from this study elucidate a novel mechanism of "virus mimicry" by which stromal-tumor cell interactions promote an anti-viral response in breast cancer cells that renders them more aggressive and resistant to treatment. The expression of RN7SL1 in stromal-derived exosomes opens up the possibility that this exoRNA could serve as a potential biomarker from liquid biopsies to predict whether a patient will respond to chemotherapy or radiation treatments. In conjunction with RN7SL1, the presence of ISGs in primary breast tumors could also be used to further predict how a patient will respond to treatment. Beyond the use of biomarkers, this work provides a strong foundation for future studies using targeted therapeutics to resensitize breast tumors to chemotherapy and radiation and ultimately reduce metastatic burden in patients.
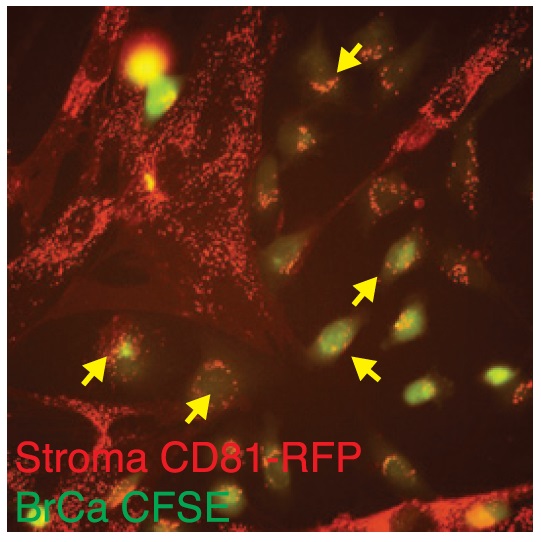
Fibroblast Exosomes.
Graphic used with the permission of Dr. Andy Minn and the University of Pennsylvania.
Graphic used with the permission of Dr. Andy Minn and the University of Pennsylvania.
Publications:
Boelens MC, Wu TJ, Nabet BY, Xu B, Qiu Y, Yoon T, Azzam DJ, Twyman-Saint Victor C, Wiemann BZ, Ishwaran H, Ter Brugge PJ, Jonkers J, Slingerland J, Minn AJ. 2014. Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell 159: 499-413.
Nabet BY, Qiu Y, Shabason JE, Wu TJ, Yoon T, Kim BC, Benci JL, DeMichele AM, Tchou J, Marcotrigiano J, and Minn AJ. 2017. Exosome RNA unshielding couples stromal activation to pattern recognition receptor signaling in cancer. Cell 170: 352-366.
Links:
Last updated Wednesday, March 12, 2025














