Consumer Involvement
Melanoma Research Program, Peer Review Consumer Reviewer




Trena Brown
(Photo Provided)
In January 2016, I was on top of the world as a Black woman who had achieved my corporate dreams. I had climbed the corporate ladder to be vice-president of one of the largest companies in the U.S., and then I happily retired. I was financially well off and could really enjoy life and travel the world. I returned to an old passion, designing and making jewelry. I even met my soul mate, and we had enjoyed one of the best years of my life together.
In February 2016, my life turned upside down. One night, I received a notification through my online health portal that I had metastatic melanoma in my lungs. How did I get to this point?
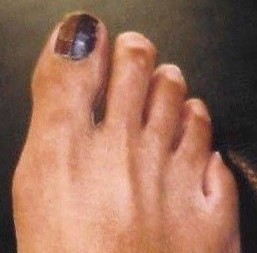
Figure 1: Photo of Trena's toe, showing how the skin under the nail had become black
(Photo Provided)
In the 1980s, I noticed brown streaks on my big, right toenail. I went to a dermatologist for treatment of what I thought must surely be a fungus. The dermatologist told me the streaks were not in the toenail, but under the nail in the skin. He told me to not worry about the streaks�that they would probably get darker as I got older, and the toenail might even turn black. That is exactly what happened (Figure 1).
Assured by the doctor there was nothing wrong, for 15 years I continued to get pedicures with extra coats of polish on that nail to hide the darkness. At one point another dermatologist noticed my dark toe, gave me a pamphlet about melanoma, and ordered a biopsy. The biopsy came back negative. Several years later, yet another biopsy did identify a pre-melanoma lesion, so I had surgery to remove the nail and clear the area. After the surgery, the margins of the removed tissue were declared clear, and I assumed the issue was resolved. I went on with my life, climbing the ladder and achieving dreams.

Figure 2: Photo of Trena's toe years after the nail was removed, showing the appearance of a brown "blister" that was later identified as melanoma (Photo Provided)
In 2013, after retiring from corporate life, I was on vacation and noticed the side of the toe had an ugly brown blister (Figure 2). It didn�t hurt, so I put on a band-aid and enjoyed my trip. When I returned home, I got another biopsy of the toe. Two days later, I heard these words, �Trena, you have melanoma, and you are going to lose your toe.� After the surgery I was informed that both my sentinel lymph node and the margins were clear. Once again, I thought the issue was resolved. Six weeks later, I began working with a trainer and exercising regularly to restore my balance and get stronger (Figure 3).

Figure 3: Photo of Trena's toe, healed from the amputation to remove the melanoma
(Photo Provided)
One day in 2015, my trainer observed that I was out of breath and she would not let me dismiss the comment, insisting that I was more out of breath than usual. Two months later, at the end of an appointment with my internist�who had just pronounced me healthy�I repeated what my trainer said about my breathing. I proceeded to get a chest X-ray, then a CT scan, and finally a lung biopsy. Unfortunately, I learned that the diagnosis was metastatic melanoma in my lungs because of an alert through MyChart. At night. Before I could talk to my doctor. My trainer had saved my life, but that life had just been turned upside down.
There was screaming and crying. I tried to learn about my condition online, where �Dr. Google� suggested I had a year to live. Doctors gave me statistics on the newly available immunotherapies, their potential side effects, and success rates. Side effects were noted as too difficult for most patients to tolerate, but I decided I was going to be in the minority.
I began a two-year treatment plan�four months of Yervoy � and OPDIVO �, followed by straight OPDIVO � every other week. There were many nights when I could not sleep due to a horrendous body rash, and many days when I was too fatigued to do much other than to get out of bed. I lost my hair and developed large, white patches on my brown face, a condition called vitiligo. I was diagnosed with hypothyroidism and adrenal insufficiency. But I was determined. I was going to finish the treatment. I dragged myself to the gym twice a week during the worst of it. Medication eventually restored both my hair and my energy. I was told the vitiligo probably would not go away, but it was a good sign the immunotherapy was working. To my delight, after four months, preliminary scans showed the tumors in my lungs had shrunk significantly. Today, I show no evidence of disease.
Looking back on my experiences, several things come to mind. The first is comprehending all the bad information that I received from multiple doctors and realizing how easily someone can get mis-diagnosed. I have learned it is crucial to be your own healthcare advocate.
Second, I am appalled by the general ignorance, including my own, regarding melanoma in Black and Brown people. We know much about cutaneous melanoma, the most common form of melanoma that is typically diagnosed in people with light skin. Yet, there is very little information or publicity about acral melanoma. It is the most common form of melanoma diagnosed in people with darker skin and is the form of melanoma that went undiagnosed in me all those years. The cause of acral melanoma is unknown, but I am doing what I can to spread awareness that it exists. I am pleased when people let me know they insisted on full body scans that discovered their melanoma early.
I did not travel this melanoma journey alone. Soon after my diagnosis, I was fortunate to be introduced to someone who worked at the Melanoma Research Alliance (MRA). At her invitation, I attended the MRA�s annual conference, where I learned about melanoma and met people who have become life-long support friends. The MRA has become a second family.
Because of my dedication to continuing education about acral melanoma, the MRA has interviewed me several times for their website and referred me to other organizations and companies for informational videos, podcast interviews, and articles. When I learned about the opportunity to become a consumer reviewer for the Melanoma Research Program (MRP), I eagerly applied and was delighted to be accepted. I was apprehensive about the material because I did not have a scientific or research background, and I had to look up many terms to understand the applications I was assigned to review. When I sat for the first all-day review and heard the critiques from the doctors who presented before me, I wondered if we had read the same grant application. But I was pleased to get positive feedback on my comments and respect for my individuality from the professionals on my panel.
I am hopeful that one of the grants we review may be the one to identify a cause of acral melanoma. I am proud to be a part of the MRP review process, and I look forward to participating again this year.
The views, opinions, and/or findings contained in this paper are those of the author(s) and should not be construed as an official Department of the Army position, policy, or decision.
Last updated Tuesday, November 12, 2024














