Reconstructive Transplant Research
Regaining independence after the world's first successful combination face and double hand transplant



Posted August 12, 2022
Dr. Daniel Ceradini, New York University School of Medicine
Dr. Eduardo Rodriguez, New York University School of Medicine
 Dr. Eduardo Rodriguez, left, and Dr. Daniel Ceradini, right, perform reconstructive surgery at the New York University School of Medicine. (Photo Provided)
Dr. Eduardo Rodriguez, left, and Dr. Daniel Ceradini, right, perform reconstructive surgery at the New York University School of Medicine. (Photo Provided)
The successful operation was supported in part by an ongoing Fiscal Year 2014 Reconstructive Transplant Research Program Research Award - Clinical Trial Option to Dr. Daniel Ceradini from New York University (NYU) School of Medicine. Dr. Ceradini and the NYU team incorporated additional coordination and planning to mitigate complications and successfully completed this extremely complex procedure. Although there have been 41 bilateral and 38 unilateral hand transplants and 47 face transplants performed worldwide,1 there had only been two prior attempts to complete a combination face and bilateral hand transplant.
In August 2020, the team at NYU, led by Dr. Eduardo Rodriguez, performed a 23-hour surgery to transplant a full face and bilateral hand allografts onto 21-year-old Joe Dimeo. Joe had been in a motor vehicle accident, which resulted in burns over 80 percent of his body, extensive scarring of the eyelids, ear, nose, and lips, and amputation of all of his fingers. In a recent publication in Plastic and Reconstructive Surgery,1 the team describes the planning and execution of this historic life-altering surgical procedure. Now, two years post-surgery, Joe is approaching functional independence, can dress and feed himself, play pool, and has resumed lifting weights, something he was passionate about pre-injury.
Following recipient and caregiver consent, the NYU team began preparations by completing rehearsals and computerized surgical planning, as well as the creation of patient-specific cutting guides and models. After 10 months, an optimal donor was identified and transferred to NYU for allograft procurement and transplantation, which occurred simultaneously in two adjacent operating rooms (Figure 1). After surgery, Joe received a triple therapy immunosuppression regime to protect against graft rejection and was monitored in the surgical intensive care unit for 45 days. Joe remained free of acute rejection for over 8 months post-surgery. Passive occupational therapy sessions, such as a therapist manipulating Joe's muscles, were initiated at postoperative day 4 to build flexibility and prevent muscle shortening or deformation. Once Joe was transferred to an acute inpatient rehabilitation facility, daily physical and occupational therapy sessions were initiated. Therapy continued on an outpatient basis five times weekly and functional outcomes have significantly improved compared to the patient's preoperative, post-injury baseline levels. Through this therapy regime, Joe has continued to improve his range of motion with his new limbs, increase strength and sensation of both the hand and face allografts. This effort demonstrates for the first time the feasibility of combination face and bilateral hand transplantation and represents the most comprehensive vascularized composite allotransplantation ever performed (Figure 2).
"The world's first successful combined face and bilateral upper extremity transplant represents a critical milestone of reconstructive transplantation," Dr. Daniel Ceradini, the Principal Investigator, said. "The vital support of the RTR facilitated the thoughtful design, execution and analysis of this case to demonstrate feasibility and safety of highly complex VCA and broaden its applications to reconstructive surgery."
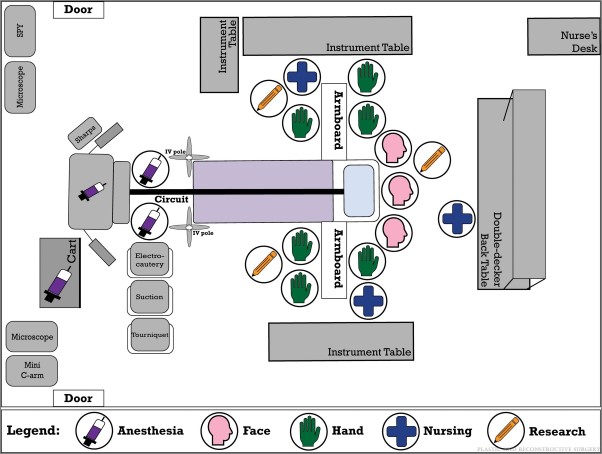
Figure 1: Schematic of operating room layout. Donor and recipient operating rooms ran concurrently, with similar organizational structure and equipment. The schematic illustrates the complexity of intraoperative personnel management. This setup was preplanned, simulated during cadaveric rehearsals, and subsequently refined based on intraoperative needs. Communication was maintained between all surgical teams and the anesthesia providers per operating room and between donor and recipient operating rooms. A research team member stationed at each surgical site facilitated procedural flow, ensured adherence to the corresponding surgical checklists and aided communication between operating rooms.
(Published with permission from and copyrights retained by Eduardo D. Rodriguez, M.D., D.D.S.)

Figure 2: Side-by-side comparison of preoperative and postoperative appearance.
The patient is pictured at presentation, left, and on posttransplant day 125, right.
(Published with permission from and copyrights retained by Eduardo D. Rodriguez, M.D., D.D.S.)
References:
1Ramly EP, Alfonso AR, Berman ZP, Diep GK, Bass JL, Catalano LW 3rd, Ceradini DJ, Choi M, Cohen OD, Flores RL, Golas AR, Hacquebord JH, Levine JP, Saadeh PB, Sharma S, Staffenberg DA, Thanik VD, Rojas A, Bernstein GL, Gelb BE, Rodriguez ED. The First Successful Combined Full Face and Bilateral Hand Transplant. Plast Reconstr Surg. 2022 Aug 1;150(2):414-428. doi: 10.1097/PRS.0000000000009369. Epub 2022 Jun 9. PMID: 35674521.
Last updated Wednesday, September 17, 2025
 An official website of the United States government
An official website of the United States government
 ) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
) or https:// means you've safely connected to the .mil website. Share sensitive information only on official, secure websites.
