Peer Reviewed Orthopaedic
Neuroma/Targeted Muscle Reinnervation Educational Highlight



Posted December 27, 2018
Featuring research by Gregory Dumanian, M.D., Northwestern University
Problem: As protective equipment and battlefield medical care continue to improve Warfighter survival following major trauma, limb amputation has become a more frequent occurrence in recent conflicts. A study done by the Congressional Research Service for the period between 2001 and 2015 indicates that 1,645 Warfighters underwent an amputation of at least one major extremity as a result of their service in an ongoing military operation during that time.1 Within the general population, an estimated 185,000 amputations are performed each year following acute trauma, such as automobile accident injuries, as well as for complications arising due to vascular diseases like diabetes and peripheral arterial disease.2 It is estimated that more than 1.7 million people in the United States are currently living with limb loss, and this number is expected to double by the year 2050.3 . In addition to the daily challenges associated with living with limb loss, some 25% of amputees develop chronic pain at the surgical site, presenting an additional challenge to achieving and maintaining a high quality of life.
Neuroma: The two most common amputation-associated pain conditions are phantom limb pain (PLP) and residual limb pain caused by a neuroma at the site of the amputation. While PLP may require a multifaceted intervention to treat, neuroma presents a specific target to improve quality of life and reduce pain. A neuroma is the result of a severed sensory or mixed sensory/motor nerve attempting to heal itself. Rather than regenerating and becoming insulated and protected in a typical myelin sheath, the nerve produces a disorganized tangle of axonal projections, Schwann cells (neuronal support cells), and perineural cells. Patients report pain when this nodular tangle of cells is mechanically stimulated through muscle contraction, movement, or touch.
Unmanaged pain caused by these neuromas is a clinical issue unto itself, but, as a consequence, the pain can also lead to reduced prosthetic device use. When the painful nodules sit at the residual limb-prosthetic interface, the contact and pressures created by their use exacerbates the neuroma-associated pain and often leads to users of prosthetics either limiting or abandoning the use of their device, and this can compromise their independence and quality of life.
Treatment Options: Treatment options for traumatic neuroma have varied over the past century, and until the 1980s there was no clinical consensus for best practice. Often, pain at the site of amputation is treated with analgesics to improve prosthetic use and quality of life. Other pain-reduction strategies include attempts to degrade or ablate the nerve with local use of neurotoxins or focused radio waves. Surgical interventions to remove the neuroma often fail to substantially improve long-term pain management, as the newly severed nerve ending simply forms a subsequent secondary neuroma. In 1984, the surgical standard of care was set after a report by Dellon and Mackinnon suggested that burying the cut end of the neuron within nearby muscle reduced the incidence of secondary neuroma formation, although a substantial fraction of patients still report pain following the procedure.4 These observations suggest that a better strategy to “cure” neuromas and alleviate pain is still needed.
PRORP Mission and Focus on Neuromas: In 2009, the Peer Reviewed Orthopaedic Research Program (PRORP) was established with funds appropriated by Congress to support research that would advance prevention, treatment, and rapid recovery of military personnel suffering from major extremity trauma. Since its inception, the PRORP has evolved to steer its research investments to address clinically relevant questions in the areas of surgical care and rehabilitation. The PRORP releases funding opportunity announcements encouraging research proposals that address military-relevant critical care gaps within the orthopaedic field. Focus Areas are recommended by the PRORP Programmatic Panel, which includes at least one consumer advocate, who is often a retired Warfighter living with an orthopaedic injury and who can speak directly to the needs of the patient community. In fiscal year 2012 (FY12) and FY14 the PRORP specifically requested applications for research that proposed “strategies to inhibit neuromas at surgical/amputation sites.” These solicitations demonstrated the Program’s understanding of the large unmet need for new approaches in pain management for amputees to increase both functionality of prosthetic devices and overall quality of life.
The PRORP has invested $11.2 million (M) in seven clinical and translational research awards that specifically address new interventions aimed at preventing or treating traumatic neuromas. These studies include laboratory concepts such as utilizing umbilical cord-derived amnion wraps to provide a regenerative environment (rather than scar formation) for crush-damaged peripheral nerves in animal models and the preclinical development of therapeutic compounds aimed at blocking the biological process of neuroma development post-amputation (OR160173, OR120168, OR160233). Additionally, the PRORP has funded studies that explore new surgical procedures, one of which is aimed at preventing or treating neuromas by implanting the newly severed nerve ending into a free skeletal muscle graft (OR160164). This approach differs from simply burying the nerve in adjacent muscle tissue, as the free skeletal muscle graft does not have a blood supply and therefore must undergo revascularization to regenerate. The severed peripheral nerve is able to properly heal in parallel with the regenerating muscle, thereby avoiding the formation of a neuroma.
In addition to these highly focused neuroma-targeted projects, the PRORP has invested an additional $8.6M in eight research awards that explore ways to regenerate peripheral nerves and/or direct their migration and integration into surviving muscle to "re-wire" the remaining limb (OR160173, OR120216). An additional award investigating targeted muscle reinnervation (TMR) following amputation was also made by the PRORP and has the potential to impact neuroma-associated morbidities for amputees as well (OR110187). Indeed, evidence from clinical outcomes following TMR-type surgical interventions suggests that these patients may experience a reduction in traumatic neuroma-associated pain following the procedure as an unintended and advantageous side-effect.
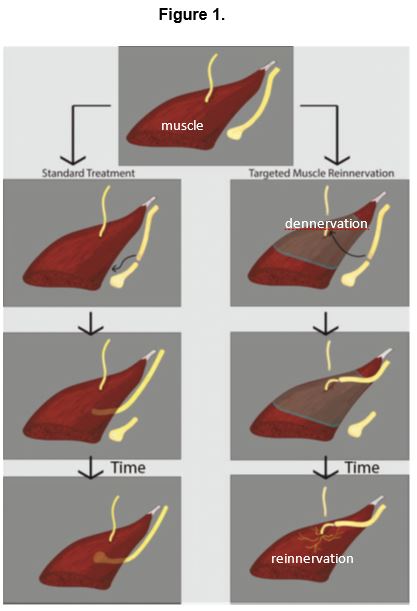
TMR: TMR is a surgical procedure, first performed in 2002, designed to amplify the signals still present in amputated nerves by reinnervating (restoring nerve function to) nearby muscles in order to control advanced myoelectric prosthetic devices.5 The surgical process (Figure 1) begins with the removal of the end-neuroma to expose healthy nerve endings of the major mixed motor/sensory nerve. An adjacent motor nerve is then cut, creating a free nerve ending that leads into a denervated muscle segment. The major mixed nerve is then transferred to the stump of the motor nerve leading into the denervated muscle segment. Upon successful reinnervation, the muscle serves to amplify the motor signals that were present in the originally amputated nerve, providing advanced prosthetic devices with new intuitive brain-controlled signals for movement.
Important clinical outcomes borne from the TMR procedure include the observation that severed motor neurons, unlike severed sensory neurons, do not appear to produce symptomatic neuromas and instead degrade, leaving the patient with no surgically induced pain as a result of the nerve being cut. Additionally, the provision of appropriate nerve receptors within the muscle gives the previously amputated nerve “somewhere to go and something to do,” and this is one theoretic mechanism by which TMR has helped individuals with neuroma pain. Also observed in these patients was the improvement in phantom limb pain, as the brain perhaps once again sensed that the end of the nerve was terminally connected.
To build on these observed clinical outcomes, Dr. Gregory Dumanian, of Northwestern University, was awarded a PRORP FY12 Clinical Trial Award based on the explicitly requested call for research proposals addressing the inhibition of neuromas (OR120021). Dr. Dumanian's team hypothesized that the reported clinical observations were more than anecdotal and that TMR would improve surgical treatment of neuromas when compared to the standard of care ‒ simply burying the affected nerve in muscle. This type of study, which compares the effectiveness of a new treatment to standard procedures, is often required in order to change clinical practice guidelines. The study team compared patient-reported pain following a surgical procedure to treat the neuroma; some patients were randomly selected to receive the standard-of-care procedure (burying the nerve in muscle) while the others received TMR. Study patients were blinded to the procedure, meaning they did not know which treatment they received.
Dr. Dumanian’s team found that PLP was significantly decreased in patients undergoing TMR one year after the procedure, while reported residual limb pain was not initially changed. However, at an 18-month final follow-up evaluation, 67% of patients receiving the TMR procedure reported mild or no pain in their limbs, compared to only 27% of patients who received standard of care. The study team suggested that those patients still perceiving limb pain may not be suffering from neuroma-associated issues but rather, may have developed heterotopic ossification, a painful bone growth defect common in amputees, which could not be accounted for in the analysis. Six of the 14 patients who received standard of care treatment have subsequently crossed over to receive the TMR procedure and have generally shown improvement in their symptoms of pain and phantoms.
The PRORP’s determination to seek and fund research in the targeted area of neuroma treatment strategies has clearly generated a dramatic return on investment with Dr. Dumanian’s findings.6 As described by Dr. Dumanian himself, these findings have engendered a rapid and widespread buzz in the surgical community as clinicians and patients hear about the results. Adopting the TMR procedure as a new standard of care for amputees reporting neuroma-associated pain appears to be long overdue. The team plans to complete their PRORP award by hosting clinician training courses to disseminate the surgical knowledge on how to perform TMR, as well as to promote the use of TMR as a pain prevention technique at the time of amputation.
References:
1 Congressional Research Services Report 2015.
3 Zeigler-Fraham K, MacKenzie EJ, Ephraim PL, Travison TG, and Brookmeyer R. 2008. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Archives of Physical Medicine and Rehabilitation 89(3):422-429.
4 Dellon AL, Mackinnon SE, and Pestronk A. 1984. Implantation of sensory nerve into muscle; preliminary clinical and experimental observations on neuroma formation. Annals of Plastic Surgery 12(1):30-40.
5 Kuiken TA, Dumanian GA, Lipschutz RD, Miller LA and Stubblefield KA. 2004. The use of targeted muscle reinnervation for improved myoelectric prosthesis control in a bilateral shoulder disarticulation amputee. Prosthetics and Orthotics International (28):245-253.
6 Dumanian GA, Potter BK, Mioton LM, Ko JA, Cheesborough JE, Souza JM, Ertl WJ, Tintle SM, Nanos GP, Valerio IL, Kuiken TA, Apkarian AV, Porter K, and Jordan SW. 2018. Targeted muscle reinnervation treats neuroma and phantom limb pain in major limb amputees – A randomized clinical trial. Annals of Surgery [Epub ahead of print].
Links:
Public and Technical Abstracts
Peripheral Nerve Repair and Prevention of Neuroma Formation
Prevention and Treatment of Neuroma and Induction of New Nerve Growth
Clinical Trials of Pattern Recognition, Electrode Grid, RIC Arm in TMR Subjects
Targeted Reinnervation as a Means to Treat Neuromas Associated with Major Limb Amputation
Last updated Monday, January 3, 2022

















