Prostate Cancer
PSMA-PET Imaging in Prostate Cancer: From Detection to Therapeutics
Innovative ideas advancing the field of PET imaging and providing breakthroughs for patients



Posted September 16, 2022
Over the past three decades, researchers have developed new approaches for using positron emission tomography (PET) to specifically detect prostate cancer by combining this nuclear imaging technique with Prostate Specific Membrane Antigen (PSMA), a surface protein with increased expression on prostate cancer cells. The results of these research efforts finally culminated in the U.S. Food and Drug Administration (FDA) approval of two first-of-its-kind PSMA-PET imaging agents for use in prostate cancer patients. In December 2020 and May 2021, 68-Ga-PSMA-11 and 18-F-DCFPyL, respectively, were approved for the detection of metastatic and/or recurrent prostate cancer. Early funding from the Prostate Cancer Research Program (PCRP) was integral to the development of the PET-PSMA field, and the PCRP’s continued funding of clinically impactful research has advanced the PSMA-PET field from detection to therapeutics.

Dr. Sandi Kwee
(Photo Provided)

Dr. Martin Pomper
(Photo Provided)
PSMA-PET: Development of a New Field: In 2004 and 2005, the PCRP funded two innovative projects that ultimately laid the groundwork for this entirely new field of imaging research. With a Fiscal Year 2004 (FY04) New Investigator Award, Dr. Sandi Kwee aimed to improve targeted radiotherapy by using PET imaging to delineate specific areas of prostate cancer. Dr. Kwee’s approach focused on using 18-F Fluorocholine, the most promising PET radiotracer for prostate cancer at that time. This early clinical research study in PET imaging of prostate cancer showed that it was feasible to apply PET tracers to localize difficult prostate cancer lesions for targeted biopsy and radiation therapy. Numerous studies and clinical trials have since followed in investigating novel PET tracers such as PSMA for planning radiation therapy and monitoring treatment response in prostate cancer. While Dr. Kwee’s research aimed at improving uptake of a new radiotracer, Dr. Martin Pomper was investigating approaches to develop small-molecule PET imaging agents that would specifically bind to prostate cancer cells, thereby improving the specificity of this approach. With an FY05 Idea Development Award, Dr. Pomper developed and tested nine new PET radiotracers that specifically target PSMA. His novel study resulted in the development of a urea-based 18F-labeled, PSMA-targeted radiotracer that showed promise for targeted PSMA-PET agents to image prostate cancer, and created a new class of agents that ultimately led to the two FDA-approved imaging agents used in the clinic today. Drs. Kwee and Pomper set the stage for PSMA-PET targeting to be used in prostate cancer and created an entirely new field of research for detection, treatment response prediction, and theranostics.
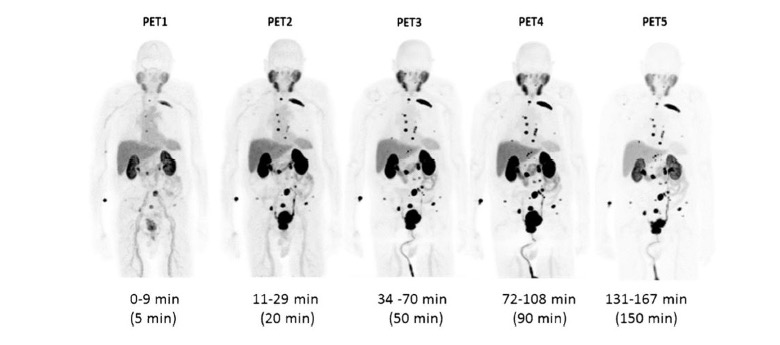 Figure 1: Maximum intensity PET (MIP) image sequence in subject #4. This patient demonstrated radiotracer binding in a large number of metastatic lesions involving multiple bones and lymph nodes.1
Figure 1: Maximum intensity PET (MIP) image sequence in subject #4. This patient demonstrated radiotracer binding in a large number of metastatic lesions involving multiple bones and lymph nodes.1 
Dr. Robert Reiter
(Photo Provided)
Dr. Anna Wu
(Photo Provided)
Expansion of the Field: PSCA-PET: The PCRP continued to receive new ideas for using PET imaging to improve prostate cancer detection and invested in other novel approaches proposed by Dr. Robert Reiter that included use of a different novel target, called Prostate Stem Cell Antigen (PSCA), which is also highly expressed on prostate cancer cells. Dr. Reiter received funding from an FY07 Laboratory-Clinical Transition Award to develop small PSCA-targeted antibody fragments for molecular imaging of prostate cancer with SPECT (Single Photon Emission Computed Tomography) and PET scans. The lead compound from this study, A11 (NCT02092948), successfully detected prostate tumors in several mouse models, warranting additional investigation. Dr. Reiter partnered with Dr. Anna Wu and received an FY14 Synergistic Idea Development Award to develop additional antibody fragments that were dually capable of PET and optical imaging. Results from the study suggested that a dually labeled anti-PSCA antibody fragment can provide noninvasive whole-body PET imaging to localize PSCA-expressing tumors, followed by fluorescent image-guided surgery to visualize tumors intraoperatively.

Dr. Henry VanBrocklin
(Photo Provided)

Dr. Andrei Iagaru
(Photo Provided)
Applications of PET for Diagnosis and Disease Monitoring: Earlier studies had demonstrated the potential of PSMA-PET imaging for detection of prostate cancer, but the specific application of this new technology was still being created. The PCRP funded additional work to investigate novel applications of PSMA-PET imaging molecules, including funding the work of Dr. Henry VanBrocklin and Dr. Andrei Iagaru. Dr. VanBrocklin received an FY13 Laboratory – Clinical Transition Award to develop and test a new PET imaging agent, CTT1057 radiolabeled with fluorine-18 to non-invasively detect and stage primary and metastatic prostate cancer without the need of a traditional biopsy. [18F]CTT1057 was studied in a phase 1 clinical trial (NCT02916537) that was completed in 2017 (Behr et al., J Nucl Med 2019, 60:910) and is currently being tested in a phase 2/3 clinical trial (NCT04838626) that is anticipated to be completed in 2023. Dr. Iagaru’s work, funded by an FY15 Impact Award, investigated 68Ga-RM2 (formerly known as DOTA bombesin or BAY 86-7548) in a PET/MRI scan to see whether it would detect recurrent prostate cancer in men with high or rising PSA after treatment, better than the standard of care. The results of this clinical trial (NCT02624518) showed that 68Ga-RM2 PET/MRI had improved detection and diagnostic accuracy compared to conventional imaging techniques, indicating a promising PET radiopharmaceutical for high-risk patients with biochemical recurrence of prostate cancer.
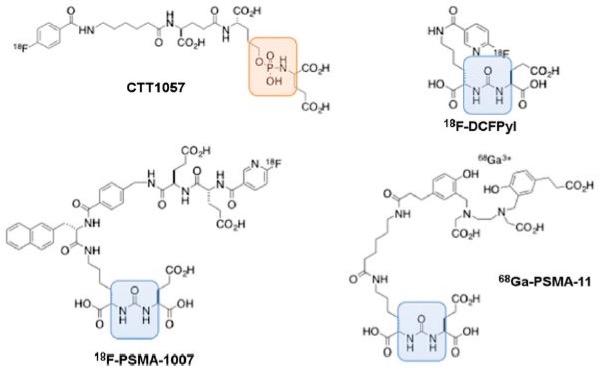 Figure 2: Chemical structure of CTT1057 with comparison to other urea-based PSMA PET agents: 18F-DCFPyL, 18F-PSMA-1007, and 68Ga-PSMA-11. Orange area highlights phosphoramidate backbone in CTT1057, and blue area highlights urea backbone in other three agents.2
Figure 2: Chemical structure of CTT1057 with comparison to other urea-based PSMA PET agents: 18F-DCFPyL, 18F-PSMA-1007, and 68Ga-PSMA-11. Orange area highlights phosphoramidate backbone in CTT1057, and blue area highlights urea backbone in other three agents.2

Dr. Rahul Aggarwal
(Photo Provided)

Dr. Michael Evans
(Photo Provided)
Applications of PET for Treatment Response Prediction: As the field continued to evolve, the PCRP funded multiple PET-imaging studies that aimed to not only detect prostate cancer, but also predict an individual’s disease progression and/or response to therapeutics. With an FY15 Idea Development Award (New Investigator Option), Dr. Rahul Aggarwal assessed the use of radiotracer 68-Gallium citrate (68-Ga) as a non-invasive biomarker of Myc activity, which, when overexpressed, can indicate treatment-resistant metastatic disease. He further explored 68-Ga citrate PET in an FY18 Idea Expansion Award to detect and monitor treatment response in treatment-emergent small-cell neuroendocrine prostate cancer, an aggressive form of PCa that is often resistant to traditional androgen deprivation therapies. This study has been integrated into an ongoing clinical trial, PROMOTE (NCT02735252), at the University of California, San Francisco, to identify predictive biomarkers for genitourinary cancers and is anticipated to be completed in 2025. Similar to Myc, glucocorticoid receptor (GR) upregulation is also associated with treatment-resistant, castrate-resistant prostate cancer (CRPC). With an FY14 Idea Development Award (New Investigator Option), Dr. Michael Evans developed a PET agent, carbon radiotracer 11C-YJH08, to target the GR, which is expected to be upregulated in mCRPC tumors to bypass treatment with androgen-signaling inhibitors like enzalutamide and abiraterone. With an FY19 Idea Expansion Award, Dr. Evans translated 11C-YJH08 and opened a phase 1 clinical trial (NCT04927663) to identify how frequently the GR-mediated mechanism occurs in mCRPC patients whose tumors have acquired resistance to androgen-signaling inhibitors. For those patients in which GR overexpression drive resistance, 11C-YJH08 PET can be applied in the future to confirm target engagement and test for early treatment responses for the numerous GR antagonists in clinical development (e.g., mifepristone, Relacorilant).

Dr. Scott Tagawa
(Photo Provided)

Dr. Michael Hofman
(Photo Provided)
Targeting PSMA for Treatment: With decades of foundational studies that demonstrated the feasibility of PSMA-targeted radiolabeled constructs, PSMA-targeted theranostics evolved. These agents target and detect cancer cells and are able to treat the disease as well. In March 2022, the FDA approved a new theranostic agent Pluvicto, 177Lu-PSMA-617, a PSMA-targeted radionuclide, from Novartis for men with metastatic CRPC. Similarly, Dr. Scott Tagawa’s Cornell team utilized the PSMA antibody J591, conjugated with radionuclides, including lutetium 177 (177Lu) and antinium 225 (225Ac), to develop new PSMA-targeted radionuclide therapies (PSMA-TRTs) that underwent phase 1 and phase 2 testing in clinical trials with a lead compound in phase 3. With an FY17 Idea Development Award (Established Investigator with Partnering Principal Investigator Option), Dr. Tagawa and his team analyzed biospecimens and clinical outcomes collected from these multiple trials to better understand a patient’s response to various PSMA-TRTs on a molecular level. Results from these sequential studies have demonstrated the safety and activity of PSMA-TRT, dose-response, association of clinical outcome with baseline PSMA imaging, and early data on resistant genotypes. Additional studies with 177Lu-PSMA-617 include an FY18 Impact Award, where Dr. Michael Hofman is investigating the combination of 177Lu-PSMA-617 with current standard-of-care chemotherapy docetaxel and androgen-deprivation therapy in men with newly diagnosed prostate cancer to improve outcomes and potentially cure patients. This phase 2 clinical trial is still currently recruiting and is anticipated to be completed in late 2022 (NCT04927663).
Since the inception of the program in FY97, the PCRP has sought innovative ideas and approaches to tackling major gaps in prostate cancer research and patient care, including the need for improved detection and new treatment options. The contributions of the PCRP enabled the discovery and development of a new field of imaging research that has led to significant advancements for the prostate cancer research and patient community, including the FDA’s approval of two new diagnostic PSMA-PET imaging agents and one theranostic agent for patients with recurrent and metastatic disease. While this represents a major step forward towards improving detection and treatment for prostate cancer patients, the PCRP will continue supporting innovative ideas that drive new clinical advancements to help the program achieve its vision of conquering prostate cancer.
References:
1Szabo, Mena, Rowe, et al. Initial Evaluation of 18F-DCFPyL for Prostate-Specific Membrane Antigen (PSMA)-Targeted PET Imaging of Prostate Cancer. Mol Imaging Biol. 2015.
2Behr, Aggarwal, VanBrocklin, et al. Phase 1 Study of CTT1057, an 18F-labeled Imaging Agent with Phosphoramidate Core Targeting Prostate-Specific Membrane Antigen in Prostate Cancer. J Nucl Med. 2019.
Links:
Sandi Kwee: Cancer Localization in the Prostate with F-18 Fluorocholine Positron Emission Tomography
Martin Pomper: PSMA-Based PET Ligands for Prostate Cancer Imaging
Robert Reiter: Development of PSCA-Targeted Minibodies for Imaging of Prostate Cancer
Last updated Thursday, September 15, 2022

















